JOINTS 2025;
3: e1572
DOI: 10.26355/joints_20258_1572
Use of weight-bearing computed tomography in knee disorders: a scoping review
Topic: New Technologies
Category: Scoping Review
Abstract
OBJECTIVE: Several studies have proven the value of weight-bearing computed tomography (WBCT) in orthopedic surgery. The purpose of this study was to review the applications of WBCT in the management of knee disorders, highlighting advantages and gaps in knowledge.
MATERIALS AND METHODS: This PRISMA-compliant systematic review, registered on the Open Science Framework, included studies in which WBCT had been used to assess patients presenting with knee ailments. The characteristics of the cohort, study design, technical details, and clinical findings at the longest follow-up were recorded. The risk of bias was assessed using the methodological items for non-randomized studies (MINORS) instrument.
RESULTS: Seventeen studies (680 knees), published from 2015 to 2025, were selected. Three studies had a prospective comparative design, 9 a retrospective comparative one and 5 were retrospective non-comparative. The conditions for which WBCT was requested were osteoarthritis (47%, 8/17), patellofemoral joint maltracking (5/17), knee malalignment (1/17) and total knee arthroplasty (3/17). Mean MINORS was 8.5/16 for non-comparative studies and 12.1/24 for comparative ones.
CONCLUSIONS: In this review, we found an increasing use of WBCT in the assessment of the most common knee pathologies. In particular, some new concepts have been introduced regarding the anatomy of the patellofemoral joint under physiological stance and the three-dimensional nature of osteoarthritis.
Introduction
Imaging plays a key role in understanding orthopedic conditions. Computed tomography (CT) scans and magnetic resonance imaging (MR) are daily requested by orthopedic surgeons as second-line imaging, being necessary to plan procedures such as osteotomies and joint replacements1,2. Until a few years ago, the only way to obtain “weight-bearing” imaging was through plain radiographs, which helped gauge the real alignment of bony segments and assess joint spaces as accurately as possible. This also provided indirect data around soft tissues and their integrity around joints3. The introduction and the diffusion of WBCT in the orthopedic arena has allowed to overcome limits inherently related to bi-dimensionality (such as bone superimposition, rotation bias, operator-related bias, etc.) enabling to get three-dimensional images in physiological stance along with a reduced amount of radiation (cone beam technology instead of traditional fan beam tomography) as compared to standard CTs4. While the initial technology was limited to feet and ankles, more recent machines have been marketed with the ability to scan the whole lower limb up to the hips. A quick look at the literature suggests that some authors have already assessed the value of WBCT in the management of knee conditions, such as osteoarthritis and patellofemoral instability.
With this background, we systematically reviewed the literature in order to determine the value of WBCT in the management of knee conditions, highlighting clinical advantages and identifying potential gaps in knowledge.
Materials and Methods
Study Protocol
This scoping review was designed according to the extension for scoping reviews of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA-ScR). The study protocol was registered on the Open Science Framework database (https://doi.org/10.17605/OSF.IO/76F59).
Eligibility Criteria
The inclusion criteria for this review were as follows: clinical studies reporting data on validated or potential applications of cone beam WBCT machines in knee pathologies, published from 2013 to 2025; prospective and retrospective cohort studies and technical notes; English-language articles; full-text availability, either online or after direct contact with the authors. Case reports, letters to the editor, instructional courses, expert opinions, laboratory studies and studies on animals were excluded. References from previous narrative or systematic reviews were analyzed and extracted if indicated.
Information Sources and Search
A systematic search was conducted on PubMed, from inception through June 15th, 2025, with the following keywords and Boolean operators: ((weight) AND (bearing) AND (ct*) AND (knee)). Additional studies were identified in the bibliographies of articles. Two reviewers (AI and AB) independently screened the results of the research, and then the full text of eligible studies was analyzed. Disputes were resolved by the senior author (AB). Unpublished studies and gray literature were not considered.
Data Charting and Items
Data were charted independently by two investigators (AI and AB) using an Excel sheet. Data were harvested regarding the cohort, the study design, and the clinical application at the latest follow-up. Results were compared in order to verify that no data was missed.
Risk of Bias
Quality assessment of both comparative and non-comparative studies was performed using the Methodological Index for Non-Randomized Studies (MINORS) criteria. This checklist covered the following eight categories to assess non-randomized controlled trials (NRCTs): clearly stated objectives, the inclusion of consecutive subjects, prospective collection of data, appropriate endpoints, unbiased assessment of the study endpoints, a follow-up period in line with study objectives, loss to follow-up less than 5% and a prospective sample size calculation4. Each of these questions can be answered with “not indicated” (0 points), “indicated but insufficient” (1 point), or “indicated and sufficient” (2 points), the global ideal score being 16 for non-comparative studies. Two investigators performed the MINORS assessment twice (AI and AB) at an interval of 10 days; then, the scores were discussed whenever a difference was present until a consensus was reached. Categorization of the MINORS scores was performed based on the previous literature as follows: “Very low” (0-4 points), “Low” (5-8 points), “Good” (9-12), and “Excellent” (13-16)4.
Synthesis of Results
Summarized data were presented as total numbers, percentages, means and ranges.
Results
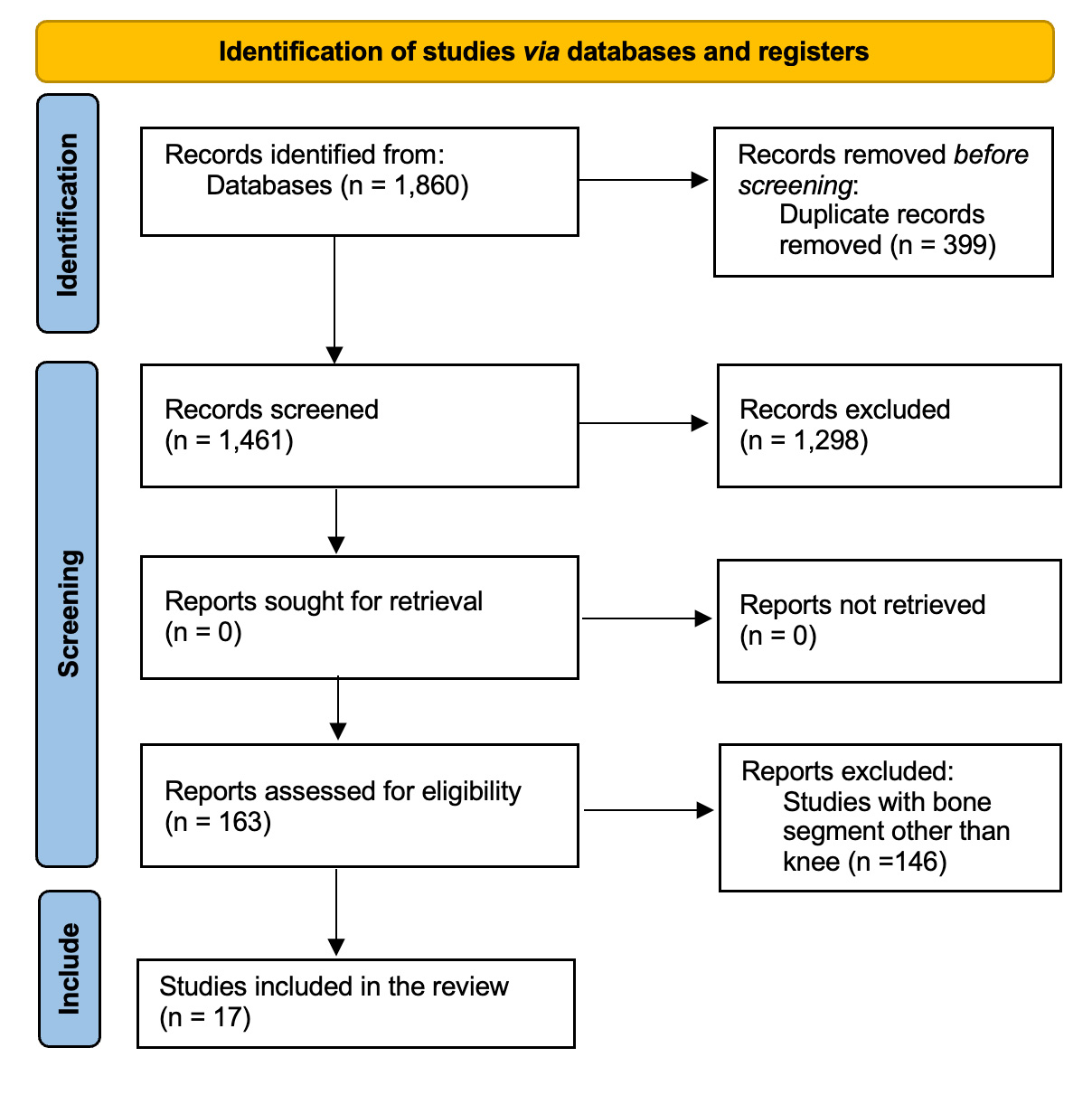
Out of 1,759 studies, 17 studies5-21 (680 knees), published from 2015 to 2025, were selected (Figure 1).
Figure 1. PRISMA 2020 flow diagram for new systematic reviews, including searches of databases and registers only.
The median year of publication was 2021 (range 2015-2025), the median sample size was 40 cases (range 10-265), with a mean age of the cohort of 49.7 ± 15 years (Table 1). Only three studies7,14,17 in this cohort were prospective comparative, nine were retrospective5,6,8,10,11,13,15,16,20 and comparative, and five9,12,18,19,21 were retrospective non-comparative. Most studies (93%) dealt with chronic conditions. Diagnostic applications of WBCT were osteoarthritis (8/17), patello-femoral joint maltracking (5/17), knee malignment (1/15), and total knee arthroplasty (3/17). The mean MINORS was 8.5/16 for non-comparative studies and 12.1/24 for comparative ones. The devices used to perform the WBCT scan are depicted in Table 2.
Table 1. Main characteristics of the studies included in this review.
| Author (year)
|
Study design | LoE | Sample Size | Minors |
| Hirschmann et al5 (2015) | Retr-Comp | III | 26 | 12 |
| Segal et al6 (2015) | Retr-Comp | III | 20 | 10 |
| Thawait et al7 (2015) | Prosp-Comp | II | 17 | 16 |
| Marzo et al8 (2016) | Retr-Comp | III | 20 | 11 |
| Hirschmann et al9 (2017) | Retr-Non Comp | IV | 10 | 11 |
| Marzo et al10 (2017) | Retr-Comp | III | 20 | 12 |
| Segal et al11 (2021) | Retr-Comp | III | 60 | 12 |
| Turmezei et al12 (2021) | Retr-Non Comp | IV | 20 | 8 |
| Lullini et al13 (2021) | Retr-Comp | III | 17 | 11 |
| Fritz et al14 (2022) | Prosp-Non Comp | IV | 26 | 11 |
| Kaneda et al15 (2022) | Retr-Comp | III | 25 | 11 |
| Sasaki et al16 (2022) | Retr-Comp | III | 43 | 12 |
| Segal et al17 (2022) | Prosp-Comp | II | 265 | 16 |
| Turmezei et al18 (2022) | Retr-Non Comp | IV | 33 | 8 |
| Buzzati et al19 (2024) | Retr-Non Comp | IV | 21 | 8 |
| Hext et al20 (2025) | Retr-Comp | III | 17 | 11 |
| Lin et al21 (2025) | Retr-Non Comp | IV | 40 | 8 |
Prosp, Prospective; Retr, Retrospective; Comp, Comparative; Non Comp, Non Comparative; LoE, Level of Evidence; Minors, Methodological Index for Non-Randomized Studies Score.
Table 2. Main findings and devices of the studies included in this review.
| Author (year)
|
Mean Age(y) | Knee
Application |
Device | Company |
| Hirschmann et al5 (2015) | 57 | Alignment | Verity | Planmed Oy |
| Segal et al6 (2015) | / | OA | Pedcat | Curvebeam AI |
| Thawait et al7 (2015) | 38.5 | OA | / | / |
| Marzo et al8 (2016) | 27.5 | Patellofemoral instability | Onsight | Carestream |
| Hirschmann et al9 (2017) | 33.7 | Patellofemoral
art |
Verity | Planmed Oy |
| Marzo et al10 (2017) | 30.5 | Patellofemoral instability | Onsight | Carestream |
| Segal et al11 (2021) | 67.6 | Patellofemoral
OA |
Onsight | Carestream |
| Turmezei et al12 (2021) | 58 | OA | Line Up | Curvebeam |
| Lullini et al13 (2021) | 21.7 | Patellofemoral
Istability |
Onsight | Carestream |
| Fritz et al14 (2022) | 55 | OA | Brilliance 64 | Philips Healthcare |
| Kaneda et al15 (2022) | 58.5 | OA | Insight | Aquilion One |
| Sasaki et al16 (2022) | / | Alignment | / | / |
| Segal et al17 (2022) | / | OA | / | CurveBeam |
| Turmezei et al18 (2022) | 57.4 | OA | Line Up | Curvebeam |
| Buzzati et al19 (2024) | 29 | Patellofemoral Instability | / | / |
| Hext et al20 (2025) | / | TKA cementless | Onsight | Carestream |
| Lin et al21 (2025) | / | TKA cementless | Onsight | Carestream |
Prosp, Prospective; Retr, Retrospective; Comp, Comparative; Non Comp, Non Comparative; OA, Osteoarthritis.
Osteoarthritis
Seven studies6,7,12,14,15,17,18 (406 knees) reported the use of WBCT to assess the joint space narrowing and the degree of knee osteoarthritis. All studies concluded that WBCT was more accurate in evaluating the joint space as compared to standard radiographic techniques and conventional CT. More specifically, Kaneda et al15 demonstrated that in the different degrees of arthritis, a greater variation in internal rotation could be observed, discussing the concept of three-dimensional arthritis15. Interestingly, in the work by Thawait et al7 a stronger correlation was found between the reduction of the medial joint space and the degree of meniscal extrusion when assessed on WBCT as compared to traditional CT images7. Regarding the progression of osteoarthritis, Segal et al6 evaluated changes in the joint space over a 24-month period, demonstrating that on images from WBCT, the amount of bone-to-bone contact could be better defined as compared to plain radiographs.
Patello Femoral Joint Maltracking
Five studies8,9,11,13,19 (148 knees) documented the application of WBCT in the assessment of the patellofemoral joint. Three studies8,9,11 evaluated the changes of patellofemoral rotation and the tibial tuberosity to trochlear groove (TTTG) distance during movement; in two8,9 of them, it was demonstrated that the TTTG and patellofemoral distance decrease with knee flexion. Segal et al11 reported a greater sensitivity and specificity of WBCT in identifying patellar cartilage changes as compared to standard radiographs. On the other side, in the study by Lullini et al13, the authors compared WBCT and traditional CT to assess the results obtained after medial patellofemoral ligament reconstruction for patellofemoral instability. They found no difference except for the TTTG distance, which was significantly reduced only on images taken in the standing position13. Finally, in the study by Buzzatti et al19, the tibial tuberosity tracheal groove distance, the bisect offset (BO), and the lateral patellar tilt (LPT) were measured in 21 healthy volunteers between 0 and 30 degrees of flexion. The authors provided important data for future studies, outlining a reference model and confirming the role of anatomical factors in patellar dislocation.
Knee Malalignment
Two studies9,16 (69 patients) investigated the role of WBCT in the assessment of knee malalignment. Hirschmann et al9 compared patellofemoral and femorotibial alignment in supine and upright weight-bearing CT, assessing the differences in terms of joint alignment. Comparing WBCT with traditional CT, femorotibial rotation changed from an external rotation in the supine position to a slight internal rotation in the upright position. The TTTG decreased significantly in WBCT, and the lateral patellar tilt angle decreased significantly in WBCT. Sasaki et al16 investigated the use of the anteroposterior axis as a reference to assess the position of the tibial component during total knee arthroplasty (TKA). They showed that the distance between the traditional and upright weight-bearing AP axis was 2.9 ± 1.6 mm at the edge of the tibial plateau. The upright non-weight-bearing AP axis was positioned in a mean of 3.5 ± 4.1 degrees of internal rotation relative to the traditional AP axis16.
Cementless TKA
Two studies20,21 (57 patients) evaluated the outcome of uncemented total knee replacement using WBCT. In the study by Hext et al20, a comparison was performed in the definition of aseptic loosening in TKA between radiostereometric analysis and WBCT analysis in the supine and loaded position at an average follow-up of 5 years. They defined an average annual migration distance for both the tibial and femoral component at 0.08 ± 0.07 mm/year and 0.18 ± 0.18 mm/year, respectively. They found a comparable accuracy in assessing the migration using the two technologies, but WBCT was proven to be more accurate in gauging the rotation of both components. In the study by Lin et al21, WBCT helped verify satisfactory stability of the prosthetic components at an average follow-up of 3 years, outlining a good reproducibility of alignment measurements as compared to standard radiology. The bone density in the different portions of the femoral and tibial components was also measured, which was identified as a clear advantage of such technology.
Discussion
The main finding of this review is that, where available, WBCT is currently being applied to assess and manage the most common conditions affecting the knee joint, with clear advantages as compared to traditional imaging techniques (i.e., plain radiographs and traditional CT). This finding aligns with a recent review22, which revealed a tenfold increase in the number of studies examining WBCT over the years 2013-2023, with a variety of conditions being investigated. However, based on the studies found in the time window between 2015 and 2025, it should be emphasized that the trend in the adoption of WBCT to assess knee pathologies is still considerably lower than what can be observed in the foot and ankle area. In our opinion, this can be explained by both the different timing of the introduction of machines able to scan the knee and the high costs of the equipment required.
Regarding the malalignment of the lower limb, there is great discussion about 3D imaging techniques as an essential tool for planning of prostheses, particularly robotic ones23. We were surprised not to find any study reporting clinical data in this setting, which may somehow be related to the limited availability of WBCT machines currently in use. We advocate comparative studies in order to demonstrate the advantage of planning arthroplasties based on images from standing CT as compared to standard CT.
As far as the patellofemoral joint is concerned, we think that the possibility to analyze distances and angles under loading conditions and different degrees of knee flexion may represent a great source of interest for researchers. Of note, in a recent paper by Ahrend et al24, the authors investigated the anatomical risk factors for recurrent dislocation using MRI images. A ruptured medial patellofemoral ligament (MPFL), a lateral trochlear index < 11°, a tibial tuberosity-trochlear groove distance (TT-TG) ≥ 16 mm, a patellar tilt > 20 mm, and an increased patellar height according to Insall-Salvati index and Caton-Dechamps index were found to be associated, although not significantly, with a higher risk of recurrent patellar dislocation. It must be remarked that such considerations were made on off-load images, and that in several studies24 reported in this review, WBCT images have demonstrated better sensitivity in defining the TTTG.
For the assessment of the joint space in knee osteoarthritis, various imaging techniques are commonly used in clinical practice, ranging from simple radiographs to 3D CT studies and MRI. Among the limitations of the CT technique, the lack of possibility of studying soft tissues is often reported, while MRI does not enable the investigation of the bone appropriately. In the recent work by Arbabi et al25, the authors evaluated the performance of synthetic computed tomography (sCT), a novel MRI-based bone visualization technique, compared with CT, for scoring knee osteoarthritis. They demonstrated that sCT and CT were comparable in this area. This demonstrates, once again, a growing interest in a three-dimensional definition of knee osteoarthritis, which takes into account the role of soft tissues and gravity stress. On a different note, two studies20,21 in this review, analyzed the role of WBCT in assessing aseptic loosening of prosthetic implants (cementless implants in both cases). Aseptic loosening represents a major cause of revision, and according to a recent review and meta-analysis by Buijs et al26, there is still great heterogeneity in terms of imaging used in the diagnostic pathway. In detail, this review demonstrates the best results in the sensitivity and specificity of MRI and Single Photon Emission Computed Tomography (SPECT)/CT, but it does not consider WBCT. It should be noted that even in this field, the margins of application of loaded CT are still to be assessed.
Some limitations have to be acknowledged in this review. We included Level III and IV studies, which are, by definition, not prospective and therefore potentially biased. Our choice at this level was dictated by the will to include all the relevant evidence produced around the application of WBCT in knee pathologies. Additionally, we did not find any study reporting the use of weight-bearing CT images in the study of post-surgical results and in traumatic conditions. Based on what we found in the current literature, we think that some limitations of WBCT devices must be considered. As an example, the initial cost of these machines has often been discussed as a potential limiting factor to the spreading of the technology in clinical centers. In this systematic research, we have not found cost-effectiveness studies that demonstrate the advantage of WBCT and support its diffusion.
Conclusions
In this review, we have found an increasing use of WBCT in the assessment of the most common knee pathologies. In particular, some new concepts have been introduced regarding the anatomy of the patellofemoral joint under physiological stance and the three-dimensional nature of osteoarthritis. Future studies are required to demonstrate clinical advantages deriving from this fascinating technology in the assessment of knee conditions.
Conflict of Interest
Authors declare no conflict of interest directly or indirectly related to this work.
Funding
This research received no external funding.
Ethics Approval and Informed Consent
Ethical review and approval were waived for this study due to the nature of the study.
AI Disclosure
No author used AI in the editing and writing of this article.
Data Availability
Data can be made available upon request to the corresponding author.
Authors’ Contributions
Conceptualization, A.B., A.I., M.D., G.M., F.L.; methodology, A.B., M.D, A.I., M.D., G.M., F.S., G.D; validation, A.B., A.I., M.D., F.L. and G.D.; formal analysis, A.B. and A.I.; data curation, A.B. and A.I.; writing–original draft preparation, A.B., A.I., M.D., G.M., G.DV., F.L.; writing–review and editing, A.B., A.I., M.D., F.L.; supervision, A.B., F.L.
All authors have agreed to the published version of the manuscript.
ORCID ID
Antonio Izzo: 0000-0001-5018-3835
Martina D’Agostino: 0009-0009-6220-7924
Francois Lintz: 0000-0002-0163-6516
Giovanni Manzi: 0000-0003-1722-3019
Alessio Bernasconi: 0000-0002-9427-3178
References
[1] Mancino F, Fontalis A, Kayani B, Magan A, Plastow R, Haddad FS. The current role of CT in total knee arthroplasty. Bone Joint J 2024; 106-B: 892-897.
[2] Aliprandi A, Perona F, Bandirali M, Randelli P, Cabitza P, Sardanelli F. MR imaging of the knee in patients with medial unicompartmental arthroplasty: comparison among sequences at 1.5 T. Radiol Med 2009; 114: 301-311.
[3] Ahmad I, Naqshband M, Nadeem A, Chaudhry DI, Akhtar M, Nadeem RD. A novel way of quantifying bone defect in primary total knee replacements using plain radiographs. J Pak Med Assoc 2023; 73: 157-161.
[4] Ekhtiari S, Horner NS, Bedi A, Ayeni OR, Khan M. The Learning Curve for the Latarjet Procedure: A Systematic Review. Orthop J Sports Med 2018; 6: 2325967118786930.
[5] Hirschmann A, Buck FM, Fucentese SF, Pfirrmann CW. Upright CT of the knee: the effect of weight-bearing on joint alignment. Eur Radiol 2015; 25: 3398-3404.
[6] Segal NA, Nevitt MC, Lynch JA, Niu J, Torner JC, Guermazi A. Diagnostic performance of 3D standing CT imaging for detection of knee osteoarthritis features. Phys Sportsmed 2015; 43: 213-220.
[7] Thawait GK, Demehri S, AlMuhit A, Zbijweski W, Yorkston J, Del Grande F, Zikria B, Carrino JA, Siewerdsen JH. Extremity cone-beam CT for evaluation of medial tibiofemoral osteoarthritis: Initial experience in imaging of the weight-bearing and non-weight-bearing knee. Eur J Radiol 2015; 84: 2564-2570.
[8] Marzo J, Kluczynski M, Notino A, Bisson L. Comparison of a Novel Weightbearing Cone Beam Computed Tomography Scanner Versus a Conventional Computed Tomography Scanner for Measuring Patellar Instability. Orthop J Sports Med 2016; 4: 2325967116673560.
[9] Hirschmann A, Buck FM, Herschel R, Pfirrmann CWA, Fucentese SF. Upright weight-bearing CT of the knee during flexion: changes of the patellofemoral and tibiofemoral articulations between 0° and 120°. Knee Surg Sports Traumatol Arthrosc 2017; 25: 853-862.
[10] Marzo JM, Kluczynski MA, Notino A, Bisson LJ. Measurement of Tibial Tuberosity-Trochlear Groove Offset Distance by Weightbearing Cone-Beam Computed Tomography Scan. Orthop J Sports Med 2017; 5: 2325967117734158.
[11] Segal NA, Murphy MT, Everist BM, Brown KD, He J, Lynch JA, Nevitt MC. Clinical value of weight-bearing CT and radiographs for detecting patellofemoral cartilage visualized by MRI in the MOST study. Osteoarthritis Cartilage 2021; 29: 1540-1548.
[12] Turmezei TD, B Low S, Rupret S, Treece GM, Gee AH, MacKay JW, Lynch JA, Poole KES, Segal NA. Quantitative Three-dimensional Assessment of Knee Joint Space Width from Weight-bearing CT. Radiology 2021; 299: 649-659.
[13] Lullini G, Belvedere C, Busacca M, Moio A, Leardini A, Caravelli S, Maccaferri B, Durante S, Zaffagnini S, Marcheggiani Muccioli GM. Weight-bearing versus conventional CT for the measurement of patellar alignment and stability in patients after surgical treatment for patellar recurrent dislocation. Radiol Med 2021; 126: 869-877.
[14] Fritz B, Fritz J, Fucentese SF, Pfirrmann CWA, Sutter R. Three-dimensional analysis for quantification of knee joint space width with weight-bearing CT: comparison with non-weight-bearing CT and weight-bearing radiography. Osteoarthritis Cartilage 2022; 30: 671-680.
[15] Kaneda K, Harato K, Oki S, Yamada Y, Nakamura M, Nagura T, Jinzaki M. Increase in tibial internal rotation due to weight-bearing is a key feature to diagnose early-stage knee osteoarthritis: a study with upright computed tomography. BMC Musculoskelet Disord 2022; 23: 253.
[16] Sasaki R, Niki Y, Kaneda K, Yamada Y, Nagura T, Nakamura M, Jinzaki M. A novel anteroposterior axis of the tibia for total knee arthroplasty: An upright weight-bearing computed tomography analysis. Knee 2022; 36: 80-86.
[17] Segal NA, Nevitt MC, Morales Aquino M, McFadden E, Ho M, Duryea J, Tolstykh I, Cheng H, He J, Lynch JA, Felson DT, Anderson DD. Improved responsiveness to change in joint space width over 24-month follow-up: comparison of 3D JSW on weight-bearing CT vs 2D JSW on radiographs in the MOST study. Osteoarthritis Cartilage 2023; 31: 406-413.
[18] Turmezei TD, Low SB, Rupret S, Treece GM, Gee AH, MacKay JW, Lynch JA, Poole KE, Segal NA. Multiparametric 3-D analysis of bone and joint space width at the knee from weight bearing computed tomography. Osteoarthr Imaging 2022; 2: 100069.
[19] Buzzatti L, Keelson B, Héréus S, Van den Broeck J, Scheerlinck T, Van Gompel G, Vandemeulebroucke J, De Mey J, Buls N, Cattrysse E. Investigating patellar motion using weight-bearing dynamic CT: normative values and morphological considerations for healthy volunteers. Eur Radiol Exp 2024; 8: 106.
[20] Hext RA, Kaptein BL, Howard JL, Lanting BA, Teeter MG. Inducible displacement of cementless total knee arthroplasty components with conventional and weight-bearing CT-based radiostereometric analysis. J Orthop Res 2025; 43: 640-649.
[21] Lin J, Zamani M, Kalia V, Vasarhelyi EM, Lanting BA, Teeter MG. Assessing implant position and bone properties after cementless total knee arthroplasty using weight-bearing computed tomography. BMC Musculoskelet Disord 2025; 26: 477.
[22] Bernasconi A, Dechir Y, Izzo A, D’Agostino M, Magliulo P, Smeraglia F, de Cesar Netto C, International Weightbearing Ct Society, Lintz F. Trends in the Use of Weightbearing Computed Tomography. J Clin Med 2024; 13: 5519.
[23] Aunan E, Alhaug E, Schuller SG, Rundfloen JE. 3-dimensional computer tomography is more accurate than traditional long-leg radiographs in the planning and evaluation of coronal alignment in total knee arthroplasty: a prospective study on 121 knees. Acta Orthop 2023; 94: 530-536.
[24] Ahrend MD, Eisenmann T, Herbst M, Gueorguiev B, Keller G, Schmidutz F, Döbele S, Schröter S, Ihle C. Increased tibial tubercle-trochlear groove and patellar height indicate a higher risk of recurrent patellar dislocation following medial reefing. Knee Surg Sports Traumatol Arthrosc 2022; 30: 1404-1413.
[25] Arbabi S, Foppen W, Gielis WP, van Stralen M, Jansen M, Arbabi V, de Jong PA, Weinans H, Seevinck P. MRI-based synthetic CT in the detection of knee osteoarthritis: Comparison with CT. J Orthop Res 2023; 41: 2530-2539.
[26] Buijs GS, Kooijenga AC, Rikken QGH, Schafroth MU, Kievit AJ, Blankevoort L. MRI and SPECT/CT demonstrate, with low certainty of evidence, the highest diagnostic accuracy for aseptic knee arthroplasty loosening: A systematic comparative diagnostic test review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2024; 32: 2061.
To cite this article
Use of weight-bearing computed tomography in knee disorders: a scoping review
JOINTS 2025;
3: e1572
DOI: 10.26355/joints_20258_1572
Publication History
Submission date: 22 Mar 2025
Revised on: 18 Jun 2025
Accepted on: 28 Jul 2025
Published online: 26 Aug 2025