JOINTS 2024;
2: e842
DOI: 10.26355/joints_20241_842
Combined anterior cruciate ligament and medial collateral ligament reconstruction results in decreased failure rates compared to non-operative treatment for grade ≥ II medial collateral ligament injuries: a systematic review
Topic: Sport Medicine
Category: Systematic Review
Abstract
OBJECTIVE: To compare patient-reported outcomes and failure rates after combined anterior cruciate ligament (ACL) and medial collateral ligament (MCL) reconstruction vs. ACL reconstruction and non-operative MCL treatment for Grade ≥ II MCL injuries at a minimum two-year follow-up.
MATERIALS AND METHODS: A literature search was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines using the PubMed, Embase, and Scopus online databases. Level of evidence I through III studies published within the last ten years (February 2013-February 2023) evaluating clinical outcomes and complications following non-operative vs. reconstruction for Grade ≥ II MCL injuries in the setting of ACL reconstruction with a minimum two-year follow-up were included. Study quality was assessed using the Cochrane risk of bias tool.
RESULTS: Five studies consisting of 236 patients were identified. Three studies (n=93 patients) reported outcomes following combined ACL-MCL reconstruction, and four studies (n=143 patients) reported results following combined ACL reconstruction and non-operative treatment for grade ≥ II MCL injury. Postoperative Tegner and Lysholm, scores ranged from 5.6 to 9, and 82.9 to 93, respectively, in the MCL reconstruction group, compared to 4.8-6.7, and 78.1-95, respectively, in the MCL non-operative group. ACL reconstruction failure rates ranged from 0% to 18.5% and 0% to 5.9% in the MCL non-operative and MCL reconstruction groups, respectively.
CONCLUSIONS: Although non-operative and reconstruction for grade ≥ II MCL injuries in the setting of ACL reconstruction both demonstrate good patient-reported Lysholm and Tegner outcome scores, higher rates of ACL reconstruction failure and chronic valgus laxity following non-operative MCL treatment were reported.
Introduction
The medial collateral ligament (MCL) and anterior cruciate ligament (ACL) share a role in stabilizing the knee against valgus force and tibial rotation1. Relatedly, ACL-MCL tears account for the most frequently combined ligament injury pattern of the knee2,3. These combined ligamentous injuries are particularly common in athletes in contact sports, such as rugby and football, due to the high energy impacts involved, as well as the propensity for direct blows to the outside of the limb, resulting in a sudden valgus force with an internal rotation moment. Despite the high incidence of these concomitant injuries, optimal treatment remains uncertain.
Historically, isolated lower-grade MCL injuries have been managed non-operatively, while grade III injuries, Stener-type lesions, bony avulsions, and those associated with chronic valgus laxity or pain have been treated operatively4. Based largely on the successful outcomes associated with non-surgical management of isolated MCL injuries reported in the literature, nonoperative treatment for the MCL in combined ACL-MCL injuries has become popular5-9. Prior investigations10,11 demonstrating successful combined ACL reconstruction with MCL bracing support this treatment strategy. However, chronic valgus instability and increased stress on the reconstructed ACL in the setting of a nonoperatively treated MCL remain a concern8,12-14. In a combined MCL grade III injury and ACL tear, in order to prevent ACL graft failure following MCL non-operative treatment, it is essential that the MCL heals completely prior to ACL reconstruction. Accordingly, no management strategy for combined ACL-MCL injuries has been agreed upon15.
Therefore, the purpose of this study was to compare patient-reported outcomes and failure rates after combined ACL and MCL reconstruction vs. ACL reconstruction and non-operative MCL treatment for Grade ≥ II MCL injuries at a minimum two-year follow-up. The authors hypothesized that both non-operative and reconstruction for MCL injuries in the setting of ACL reconstruction would result in improved clinical outcomes with a higher failure rate among the non-operative MCL treatment group.
Materials and Methods
Search Criteria and Article Identification
A systematic review was performed in accordance with the 2020 Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines. A literature search was conducted using the PubMed, Embase, and Scopus online databases on February 21st, 2023. The search included the following search terms combined with Boolean operators: “medial collateral ligament”, “anterior cruciate ligament”, “reconstruction”, “repair”, “knee”, “posterior medial corner”, “multi-ligament injury”. Inclusion criteria consisted of Level I-III human clinical studies published within the last 10 years (February 2013-February 2023) evaluating clinical outcomes and complications following non-operative vs. reconstruction for Grade ≥ II MCL injuries in the setting of ACLR with a minimum two-year follow-up. The rationale behind this temporal criterion was rooted in the evolution of surgical techniques over the years. Before 2013, there were significant changes in the approach to ACL and MCL injuries, including modifications in surgical procedures and rehabilitation protocols. To ensure that our systematic review reflects the most current and relevant evidence, we chose to focus on studies published from 2013 onwards. This approach allowed us to capture the contemporary landscape of ACL and MCL management, considering the latest surgical techniques and rehabilitation strategies that may not have been adequately represented in earlier literature. By restricting our inclusion criteria to post-2013 studies, we aimed to provide a comprehensive and up-to-date synthesis of the available evidence, thus enhancing the clinical relevance and applicability of our findings. Cadaveric studies, animal studies, case reports, registry data studies, review commentaries, letters to the editor, studies including grade I MCL injuries, MCL repair studies, studies with a minimum follow-up lower than two years, and articles not written in English-language or with English translation were excluded. Additionally, studies not reporting outcomes or failing to separate outcomes based on patients treated for grade ≥ II MCL injury in the setting of ACLR were also excluded.
Data Extraction and Outcome Measures
Two authors (C.C., D.S.) performed the data extraction from the included articles. The collected data consisted of the following: study title, first author, publication year, level of evidence, patient demographics (age, sex), mean follow-up time, MCL injury grade, MCL treatment (non-operative, reconstruction), patient-reported outcome scores (Lysholm, and Tegner), as well as the incidence of postoperative arthrofibrosis, grade II valgus laxity, and ACLR failure. ACLR failure was defined by the re-rupture of the graft.
Risk of Bias Assessment
The risk of bias for the included studies was calculated by two independent authors (C.C., S.A.) using the Modified Coleman Methodology Score. This score assesses the study quality using 10 criteria, with a score ranging from 0 to 100. A score of 100 represents a study that avoids confounding factors, bias, and chance.
Statistical Analysis
Data were qualitatively compared, and pooling was avoided due to the high risk of bias within the included studies. Due to the heterogeneity among studies and the diversity in statistical reporting, a formal meta-analysis for determining statistical significance was not performed. Box-and-whisker plots were created using Microsoft Excel version 16.63 (Microsoft Corp, Redmond, WA, USA) to illustrate the mean postoperative Lysholm, and Tegner scores for studies that reported both mean and standard deviation.
Results
Study Participants
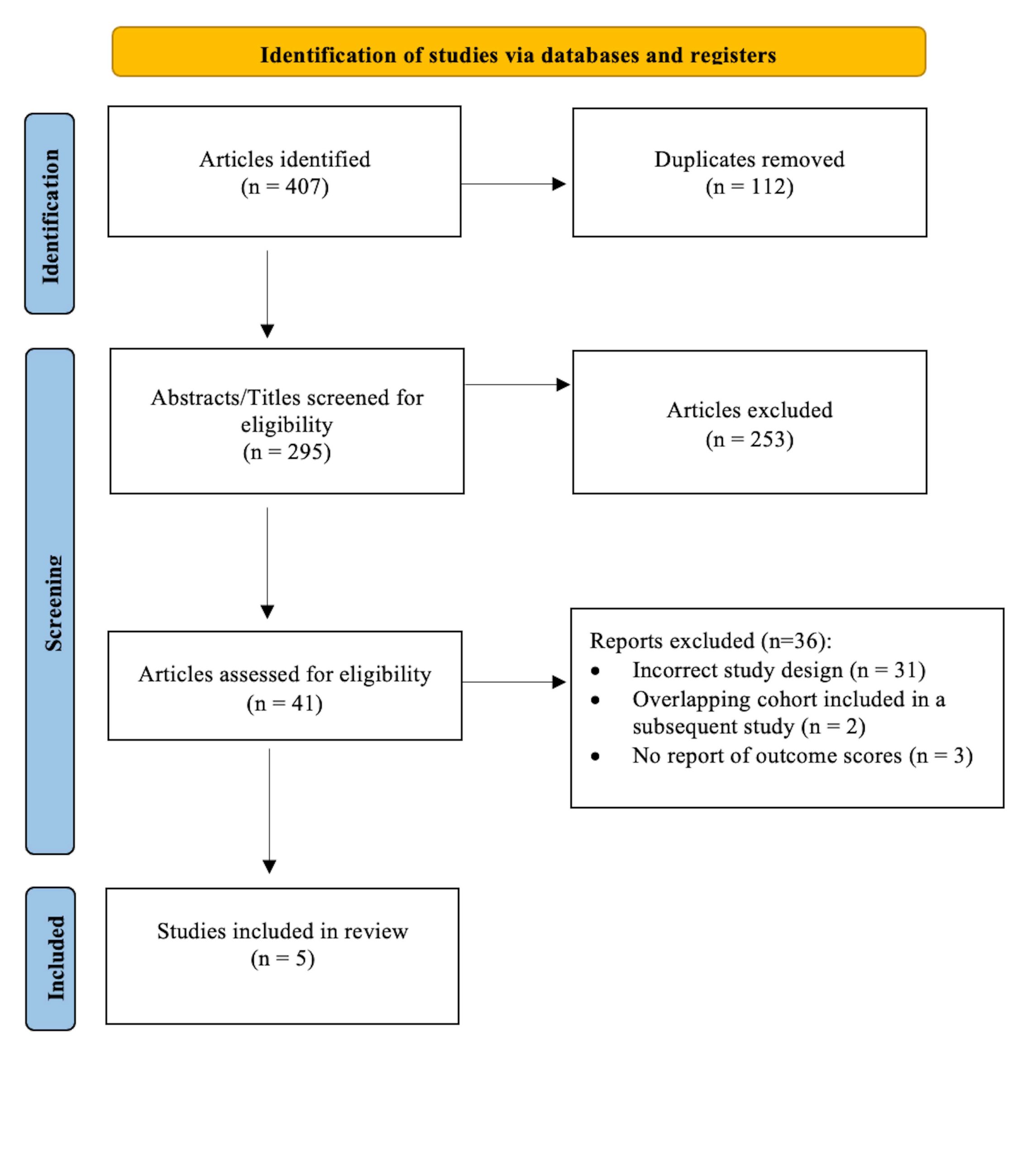
The initial search returned 407 articles. Following a screening of titles and abstracts, 41 full-text articles were evaluated for eligibility (Figure 1). Following the full-text screening and data extraction, five studies2,16-19 (n=7 cohorts), consisting of a total of 236 patients, meeting the inclusion/exclusion criteria were identified. Three studies2,16,19 (n=3 cohorts; n=93 patients) reported on reconstruction for grade ≥ II MCL injury (mean age range: 29.7-34.6 years), and four studies2,16-18 (n=4 cohorts; n=143 patients) reported on non-operative management of MCL injury (mean age range: 24.9-48.1 years). The modified Coleman score ranged from 72 to 97.
Figure 1. Preferred Reporting Items for Systematic Review and Meta-Analysis diagram of the included studies.
In the studies2,16,19 reporting on the reconstruction of MCL injury, 75 patients had grade II MCL injury, and 18 patients had MCL grade III injury. In studies2,16-18 reporting on non-operative management of MCL injury, 71 patients had grade II MCL injury, and 72 patients had MCL grade III injury. All patients underwent concomitant ACLR. One study2 was LOE I, and four studies16-19 were LOE III (Table 1).
Table 1. Patient demographics.
| Authors | LOE | Mean follow-up, mo | Mean age, yr | No. of patients | Sex (M/F) | MCL injury grade | Modified Coleman Score |
| MCL reconstruction | |||||||
| Funchal et al2 | I | 24 | 29.7 | 58 | 45/13 | II | 97 |
| Alm et al19 | III | 27.2 ± 2.8 (24-34) | 34.6 ± 13.2 (18-61) | 17 | 10/7 | II | 88 |
| Ochiai et al16 | III | 24 | 31.3 (14–69) | 18 | 11/7 | III | 72 |
| MCL non-operative treatment | |||||||
| Funchal et al2 | I | 24 | 32.5 | 54 | 42/12 | II | 97 |
| Ochiai et al16 | III | 24 | 29 (13-53) | 31 | 17/14 | III | 72 |
| Lucidi et al17 | III | 175.2 (169.2-182.4) | 48.1 ± 10.2 | 17 | 16/1 | II | 92 |
| Chen et al18 | III | 15.5 (11-27) | 24.9 (25-51) | 41 | 24/17 | III | 87 |
LOE, level of evidence; No., number; ys, years; mo, months; M, Male; F, female; MCL, medial collateral ligament; PLT, peroneus longus tendon; HT, hamstring tendon; NR, not reported.
Patient-Reported Clinical Outcome Scores
All five studies2,16-19 (n=7 cohorts; n=236 patients) consisting of 93 patients treated with MCL reconstruction and 143 patients with MCL injury treated non-operatively reported postoperative Lysholm scores (Figure 2). The reported mean postoperative Lysholm score within the MCL reconstruction patients ranged from 82.9 to 93, vs. 78.1 to 95 following the MCL non-operatively treated patients. Three studies2,17,19 (n=4 cohorts; n=146 patients) consisting of 75 patients treated with MCL reconstruction and 71 patients with MCL tears treated non-operatively reported postoperative Tegner scores (Figure 3). The reported mean postoperative Tegner score within the MCL reconstruction patients ranged from 5.6 to 9, vs. 4.8-6.7 following the MCL non-operatively treated patients (Table 2).
Figure 2. Box-and-whisker plot illustrating the mean Lysholm scores.
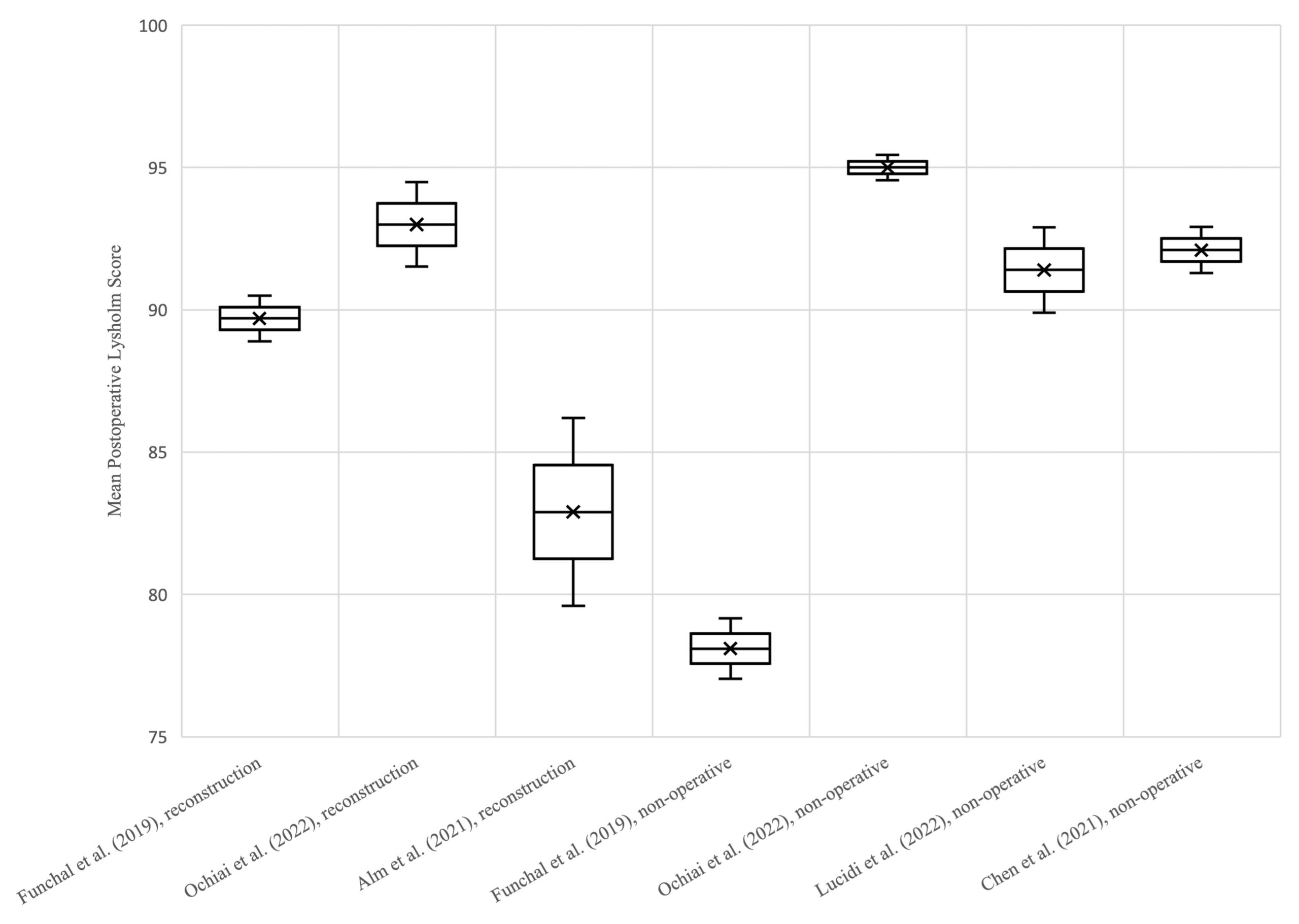
Figure 3. Box-and-whisker plot illustrating the mean postoperative Tegner scores.
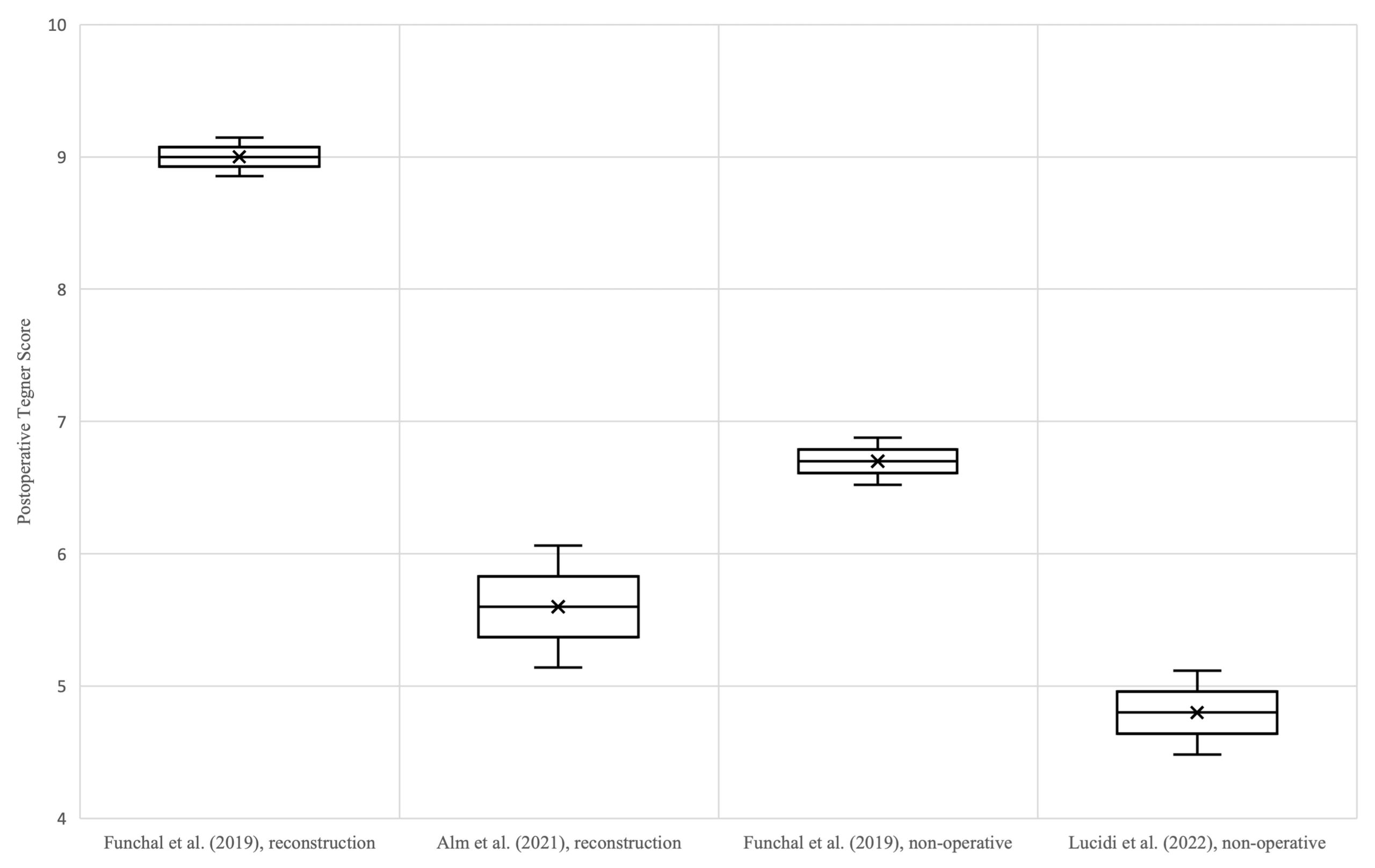
Table 2. Postoperative outcome scores.
| Authors | Lysholm | Tegner |
| MCL reconstruction | ||
| Funchal et al2 | 89.7 ± 6.1 (73-96) | 9 ± 1.1 (6-10) |
| Ochiai et al16 | 93 ± 6.3 (75-100) | NR |
| Alm et al19 | 82.9 ± 13.6 (41-100) | 5.6 ± 1.9 (3-9) |
| MCL non-operative treatment | ||
| Funchal et al2 | 78.1 ± 7.8 (54-85) | 6.7 ± 1.3 (1-8) |
| Ochiai et al16 | 95 ± 2.5 (90-100) | NR |
| Lucidi et al17 | 91.4 ± 6.2 | 4.8 ± 1.3 |
| Chen et al18 | 92.1 ± 5.2 | NR |
PLT, peroneus longus tendon; HT, hamstring tendon; NR, not reported; MCL, medial collateral ligament.
Failure Rates, Chronic Valgus Laxity, and Postoperative Arthrofibrosis
ACLR failure rates ranged from 0% to 18.5% and from 0% to 5.9% in the MCL non-operative and reconstruction groups, respectively (Table 3). Three studies2,18,19 (n=4 cohorts; n=170 patients) consisting of 75 patients treated with MCL reconstruction and 95 patients with MCL injury treated non-operatively reported the presence or absence of residual valgus laxity. Residual grade II valgus laxity at final follow-up was reported in 0-5.9% of patients within the MCL reconstruction group and 0-24.1% of patients within the MCL non-operatively treated group. No patients in either group reported postoperative arthrofibrosis.
Table 3. Postoperative arthrofibrosis, valgus laxity, and failure rates.
| Authors | ACLR failure, % | Arthrofibrosis, % | Residual grade II valgus laxity, % |
| MCL reconstruction | |||
| Funchal et al2 | 3.4 (n=2/58) | 0 | 0 |
| Alm et al19 | 5.9 (n=1/17) | 0 | 5.9 (n=1/17) |
| Ochiai et al16 | 0 | 0 | NR |
| MCL non-operative treatment | |||
| Funchal et al2 | 18.5 (n=10/54) | 0 | 24.1 (n=13/54) |
| Ochiai et al16 | 0 | 0 | NR |
| Lucidi et al17 | 5.9 (n=1/17) | 0 | NR |
| Chen et al18 | 0 | 0 | 2.4 (n=1/41) |
ACLR, anterior cruciate ligament reconstruction; NR, not reported; PLT, peroneus longus tendon; HT, hamstring tendon; MCL, medial collateral ligament.
Discussion
The most important findings from the current review were that grade ≥ II MCL injuries treated conservatively or with reconstruction in the setting of ACLR were reported to result in good clinical outcomes, although MCL reconstruction was associated with lower rates of ACLR graft failure and chronic valgus laxity. Reported rates of arthrofibrosis were zero for both treatment types. These findings suggest that grade ≥ II MCL injuries in the setting of ACL reconstruction should be managed with reconstruction to decrease the risk of ongoing instability or risk of surgical failure.
Failure rates following combined ACLR and MCL treatment were higher in patients with nonoperatively treated MCLs. These findings are similar to those reported by Svantesson et al20 in a 2019 retrospective review of the Swedish National Knee Ligament Registry, which found an increased rate of ACL revision surgery in patients with non-operatively treated MCL injuries (4.0%; n=26/657) compared to those that underwent MCL reconstruction (1.2%; n=1/84) at five-year follow-up. Although isolated MCL injuries have a high propensity to heal without surgical intervention, especially for those torn off the femur (meniscofemoral injuries), nonoperatively managed MCL injuries may not be able to assist the ACL in resisting valgus and internal rotation forces. As demonstrated by Battaglia et al13 in a 2009 cadaver study, partial and complete MCL tears resulted in significantly increased load on the ACL while resisting anterior and valgus force and internal rotational torque. A 2018 cadaver study by Zhu et al12 similarly found MCL injuries resulted in significantly increased forces on a reconstructed ACL graft; however, adding an MCL reconstruction decreased the additional forces on the ACL graft, protecting the reconstruction. Clinical application of these time-zero biomechanical results can be challenging, as comparisons are limited to ACL load in the setting of MCL tears vs. MCL reconstruction, not MCL reconstruction vs. healed tears. However, the commensurate rate of chronic valgus laxity found in this review may suggest that in the setting of combined injuries, a nonoperatively treated MCL has a lower likelihood of functional recovery, with a lower ability to offload the ACLR, putting it at risk.
Despite the difference in failure rates, PROs were similar between MCL reconstructed and nonoperatively treated MCL tear patients in the ACLR setting. This slightly contrasts previous studies20,21, which found nonoperative MCL tear treatment resulted in marginally higher and/or non-significantly higher total Knee Injury and Osteoarthritis Outcome Scores (KOOS). Interestingly, both Svantesson et al20 and Westermann et al21 found the largest difference between MCLs reconstructed and nonoperatively treated to be in the KOOS sports subscale component, with the nonoperative group performing better. This is key to informed decision-making for both patients and providers because it is possible that the additional surgery associated with an MCL reconstruction may impair a patient’s ability to return to sport. This consideration must be counterbalanced by the relatively higher risk of failure with nonoperative treatment. Although it was not demonstrated in the current study, which found no reported instances of arthrofibrosis, it is theorized12,21 that the often-reported increased risk of arthrofibrosis and stiffness associated with MCL reconstruction (or any additional knee surgery) may, in part, be responsible for the discrepancy between improved failure rates, but equivalent PRO scores found in the current review.
Rates of arthrofibrosis were equivalent in the MCL reconstruction group compared to the nonoperative group in the current review. This is in concordance with a recent 2022 prospectively randomized control trial by LaPrade et al22, comparing MCL reconstruction vs. MCL with augmented repair, which found that zero of the included 54 patients had postoperative arthrofibrosis. Conversely, older investigations, including ones by Noyes et al23 in 2000 and by Shelbourne and Porter24 in 1992, comparing MCL repair with nonoperative MCL management in the setting of ACLR, found significantly increased rates of arthrofibrosis in the nonoperative group. More recently, a study comparing (primarily) MCL repair with nonoperative treatment in the setting of ACLR by Westermann et al21 did find a higher reoperation rate for arthrofibrosis in the MCL repair group (18.8% vs. 9%), though the difference did not reach statistical significance, likely due to the relatively limited sample size. It is unclear if the contrast with the results of the current study is due to the difference in operative technique for the MCL (reconstruction in the present systematic review vs. repair in the aforementioned studies) or due to improvement in postoperative rehabilitation methods over time (when compared to the results of the abovementioned studies23,24). Accordingly, patients should still be cautioned about the risk of arthrofibrosis following MCLR, although this risk may be lower than previously thought when an anatomic MCL reconstruction is performed.
Other factors that are often utilized by clinicians to help determine operative vs. nonoperative MCL management in the setting of ACLR include tear location (proximal vs. distal), timing of MCL treatment (acute vs. delayed), and valgus gapping in full knee extension. Unfortunately, these specific variables could not be appropriately analyzed in the current review, because they were not consistently reported in the included studies. While neither variable was found to affect PROs or failure rates in the study by Westermann et al21, an older study by Nakamura et al25 did find lower rates of healing with distal MCL grade III injuries compared to proximal ones. While challenging to evaluate due to the relatively low incidence of grade III injuries, future studies evaluating the role of tear location and timing of treatment are warranted.
Despite the equivalent PROs following combined ACL reconstruction and non-operative treatment for MCL injuries found in the current review, the findings of the current study support the recent consensus statement of the Ligament Injury Committee of the German Society26 where >80% of Committee Members agreed on combined ACL-MCL reconstruction irrespective of MCL injury location such as tibial insertion, femoral insertion or mid-substance tears. However, even if it were to be agreed upon that grade III MCL injuries should be treated operatively in the setting of ACLR, it can be challenging to properly grade an MCL injury based on a physical exam alone in the context of a multi-ligament knee injury. Objective metrics of instability, such as stress radiographs, may be one way to better help characterize injury and standardize treatment27.
Limitations
The current study is not without limitations. Due to the inclusion of Level III evidence studies, pooled data were avoided, thus precluding a meta-analysis and statistical comparison. Additionally, concomitant procedures introduce confounding variables likely affecting the outcomes within this study. Furthermore, many studies did not distinguish the ACLR technique used, which subsequently may have affected the outcome scores and failure rates independently of the MCL treatment provided within the included studies. Lastly, the search strategy and inclusion criteria utilized may have unintentionally excluded studies whose data would have strengthened the current analysis.
Conclusions
Although non-operative and reconstruction for grade ≥ II MCL injuries in the setting of ACL reconstruction both demonstrated good patient-reported Lysholm and Tegner outcome scores, higher rates of ACL reconstruction failure and chronic valgus laxity following non-operative MCL treatment were reported.
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
Open access funding was provided by the Magna Graecia University of Catanzaro within the CRUI-CARE Agreement.
Informed Consent
Not applicable.
Authors’ Contributions
Substantial conception/design of work, (G.R.J., D.J.K., and J.C.), data collection (G.R.J., D.J.K., F.F., C.C.M., and D.S.), statistical analysis (S.A. and S.A.), interpretation of data (G.R.J., D.M.K., and F.F.), drafting the work (G.R.J. and D.J.K.), critically revising the work (N.N.V., R.F.L., and J.C.), manuscript preparation (G.R.J., F.F., and J.C.), approving final version for publication (all authors), and agreement for accountability of all aspects of work (all authors). All authors have read and approved the final submitted manuscript.
Ethics Approval
Not applicable.
References
- Warren RF, Marshall JL. Injuries of the anterior cruciate and medial collateral ligaments of the knee. A retrospective analysis of clinical records–part I. Clin Orthop Relat Res 1978; 136: 191-197.
- Funchal LFZ, Astur DC, Ortiz R, Cohen M. The Presence of the Arthroscopic “Floating Meniscus” Sign as an Indicator for Surgical Intervention in Patients With Combined Anterior Cruciate Ligament and Grade II Medial Collateral Ligament Injury. Arthroscopy 2019; 35: 930-937.
- Ateschrang A, Döbele S, Freude T, Stöckle U, Schröter S, Kraus TM. Acute MCL and ACL injuries: first results of minimal-invasive MCL ligament bracing with combined ACL single-bundle reconstruction. Arch Orthop Trauma Surg 2016; 136: 1265-1272.
- Kannus P. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res 1988; 226: 103-112.
- Grant JA, Tannenbaum E, Miller BS, Bedi A. Treatment of combined complete tears of the anterior cruciate and medial collateral ligaments. Arthroscopy 2012; 28: 110-122.
- Halinen J, Lindahl J, Hirvensalo E. Range of motion and quadriceps muscle power after early surgical treatment of acute combined anterior cruciate and grade-III medial collateral ligament injuries. A prospective randomized study. J Bone Joint Surg Am 2009; 91: 1305-1312.
- Millett PJ, Pennock AT, Sterett WI, Steadman JR. Early ACL reconstruction in combined ACL-MCL injuries. J Knee Surg 2004; 17: 94-98.
- Wijdicks CA, Griffith CJ, Johansen S, Engebretsen L, LaPrade RF. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am 2010; 92: 1266-1280.
- Zaffagnini S, Bonanzinga T, Marcheggiani Muccioli GM, Giordano G, Bruni D, Bignozzi S, Lopomo N, Marcacci M. Does chronic medial collateral ligament laxity influence the outcome of anterior cruciate ligament reconstruction?: a prospective evaluation with a minimum three-year follow-up. J Bone Joint Surg Br 2011; 93: 1060-1064.
- Noyes FR, Barber-Westin SD. The treatment of acute combined ruptures of the anterior cruciate and medial ligaments of the knee. Am J Sports Med 1995; 23: 380-389.
- Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med 2006; 34: 1134-1140.
- Zhu J, Dong J, Marshall B, Linde MA, Smolinski P, Fu FH. Medial collateral ligament reconstruction is necessary to restore anterior stability with anterior cruciate and medial collateral ligament injury. Knee Surg Sports Traumatol Arthrosc 2018; 26: 550-557.
- Battaglia MJ 2nd, Lenhoff MW, Ehteshami JR, Lyman S, Provencher MT, Wickiewicz TL, Warren RF. Medial collateral ligament injuries and subsequent load on the anterior cruciate ligament: a biomechanical evaluation in a cadaveric model. Am J Sports Med 2009; 37: 305-311. https://pubmed.ncbi.nlm.nih.gov/19098154/
- Mancini EJ, Kohen R, Esquivel AO, Cracchiolo AM, Lemos SE. Comparison of ACL Strain in the MCL-Deficient and MCL-Reconstructed Knee During Simulated Landing in a Cadaveric Model. Am J Sports Med 2017; 45: 1090-1094.
- Braaten JA, Banovetz MT, Rodriguez AN, Thomas P, LaPrade RF. From Anatomy to Complex Reconstruction: A Modern Review on the Medial Collateral Ligament of the Knee. Arch Bone Jt Surg 2022; 10: 818-826. https://pubmed.ncbi.nlm.nih.gov/36452420/
- Ochiai S, Hagino T, Senga S, Yamashita T, Ando T, Taniguchi N, Haro H. Analysis of Health-Related Quality of Life and Clinical Evaluations in Patients with the Triad of Combined Knee Injuries. J Knee Surg 2023; 36: 1164-1170. https://pubmed.ncbi.nlm.nih.gov/35817058/
- Lucidi GA, Agostinone P, Grassi A, Di Paolo S, Dal Fabbro G, Bonanzinga T, Zaffagnini S. Do Clinical Outcomes and Failure Rates Differ in Patients With Combined ACL and Grade 2 MCL Tears Versus Isolated ACL Tears?: A Prospective Study With 14-Year Follow-up. Orthop J Sports Med 2022; 10: 23259671211047860.
- Chen LX, Wang HH. Comparison between single- and double-bundle anterior cruciate ligament reconstructions for knee with grade 2 medial collateral ligament injury. Medicine (Baltimore) 2021; 100: e24846.
- Alm L, Drenck TC, Frings J, Krause M, Korthaus A, Krukenberg A, Frosch KH, Akoto R. Lower Failure Rates and Improved Patient Outcome Due to Reconstruction of the MCL and Revision ACL Reconstruction in Chronic Medial Knee Instability. Orthop J Sports Med 2021; 9: 2325967121989312.
- Svantesson E, Hamrin Senorski E, Alentorn-Geli E, Westin O, Sundemo D, Grassi A, Čustović S, Samuelsson K. Increased risk of ACL revision with non-surgical treatment of a concomitant medial collateral ligament injury: a study on 19,457 patients from the Swedish National Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc 2019; 27: 2450-2459.
- Westermann RW, Spindler KP, Huston LJ, Group MK, Wolf BR. Outcomes of Grade III Medial Collateral Ligament Injuries Treated Concurrently With Anterior Cruciate Ligament Reconstruction: A Multicenter Study. Arthroscopy 2019; 35: 1466-1472.
- LaPrade RF, DePhillipo NN, Dornan GJ, Kennedy MI, Cram TR, Dekker TJ, Strauss MJ, Engebretsen L, Lind M. Comparative Outcomes Occur After Superficial Medial Collateral Ligament Augmented Repair vs Reconstruction: A Prospective Multicenter Randomized Controlled Equivalence Trial. Am J Sports Med 2022; 50: 968-976.
- Noyes FR, Berrios-Torres S, Barber-Westin SD, Heckmann TP. Prevention of permanent arthrofibrosis after anterior cruciate ligament reconstruction alone or combined with associated procedures: a prospective study in 443 knees. Knee Surg Sports Traumatol Arthrosc 2000; 8: 196-206.
- Shelbourne KD, Porter DA. Anterior cruciate ligament-medial collateral ligament injury: nonoperative management of medial collateral ligament tears with anterior cruciate ligament reconstruction. A preliminary report. Am J Sports Med 1992; 20: 283-286.
- Nakamura N, Horibe S, Toritsuka Y, Mitsuoka T, Yoshikawa H, Shino K. Acute grade III medial collateral ligament injury of the knee associated with anterior cruciate ligament tear. The usefulness of magnetic resonance imaging in determining a treatment regimen. Am J Sports Med 2003; 31: 261-267.
- Guenther D, Pfeiffer T, Petersen W, Imhoff A, Herbort M, Achtnich A, Stein T, Kittl C, Schoepp C, Akoto R, Höher J, Scheffler S, Stöhr A, Stoffels T, Mehl J, Jung T, Ellermann A, Eberle C, Vernacchia C, Lutz P, Krause M, Mengis N, Müller PE, Patt T, Best R. Treatment of Combined Injuries to the ACL and the MCL Complex: A Consensus Statement of the Ligament Injury Committee of the German Knee Society (DKG). Orthop J Sports Med 2021; 9: 23259671211050929.
- Laprade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med 2010; 38: 330-338.
To cite this article
Combined anterior cruciate ligament and medial collateral ligament reconstruction results in decreased failure rates compared to non-operative treatment for grade ≥ II medial collateral ligament injuries: a systematic review
JOINTS 2024;
2: e842
DOI: 10.26355/joints_20241_842
Publication History
Submission date: 07 Nov 2023
Revised on: 17 Nov 2023
Accepted on: 17 Jan 2024
Published online: 25 Jan 2024