JOINTS 2023;
1: e632
DOI: 10.26355/joints_20236_632
What level of constraint for total knee arthroplasty in patients with poliomyelitis: a systematic review
Topic: Knee
Category: Original article
Abstract
OBJECTIVE: The aim of this article is to review the available literature on Total Knee Arthroplasty (TKA) in patients with poliomyelitis and to investigate the main approaches to this complex surgery.MATERIALS AND METHODS: A comprehensive search of PubMed, Medline, CINAHL, Cochrane, Embase, and Google Scholar databases was performed, covering the period 1988-2022 and using various combinations of the following keywords: “total knee arthroplasty”, “tka”, “total knee replacement”, “tkr”, “poliomyelitis” and “polio”.
RESULTS: Seven studies were included involving 87 patients with poliomyelitis undergoing primary total knee arthroplasty with a mean follow-up of 66 months. Good pain relief and functional outcomes have been reported.
CONCLUSIONS: The limited quantity and quality of the relevant literature are insufficient for a meaningful statistical analysis. However good pain relief and functional outcome have been reported by several authors, especially the ones suggesting a more constrained implant providing intrinsic stability.
Introduction
Poliomyelitis is the result of a viral infection attacking the anterior horn cells of the spinal cord that control the skeletal muscle cells of the trunk and limbs. The infection of these cells accounts for the diffuse severe paralysis seen with the initial infection. Muscle weakness is the clinical hallmark of patients with sequelae of poliomyelitis. This lower motor neuron disease can lead to poor motor control affecting one or both lower extremities with possible progressive deformities of weight-bearing joints and the development of osteoarthritis. Acute poliomyelitis has become a rare condition and the disease has been virtually eliminated in most of the world as a result of effective immunization programs. However, patients who had suffered poliomyelitis are now in an age range for degenerative joint disease and arthritis1.
Knee arthroplasty in these patients is complicated by some critical bone and soft tissue abnormalities around the knee, such as poor bone quality, ligament laxity, axial and rotational deviation, impaired motor control and muscular strength. As a result of all these conditions, patients present severe deformities and grossly unstable joints. The surgery is highly demanding and requires a careful preoperative assessment to determine the correct surgical indication, technique and choice of the proper implant. The severe deformities often lead to impaired exposure during surgery, therefore additional techniques are sometimes necessary, such as lateral retinacular release, medial soft-tissue release, quadriceps snip and even osteotomy of the tibial tubercle2. In addition, the low degree of stability of the native knee and the inability to restore it with conventional TKA designs, have pushed some orthopedic surgeons to consider more constrained implants as first implant of choice, especially in patients with poor quadriceps strength to provide intrinsic stability because of the increased risk of recurrence of hyperextension and ligamentous laxity3.
The aim of this article is to review the available literature on Total Knee Arthroplasty (TKA) in patients with poliomyelitis and to investigate whether different authors’ approach in the management of these challenging patients influences the outcomes4.
Materials and Methods
The current systematic review has been carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement5. The corresponding flow diagram can be found in Figure 1.
Figure 1. PRISMA flow diagram.
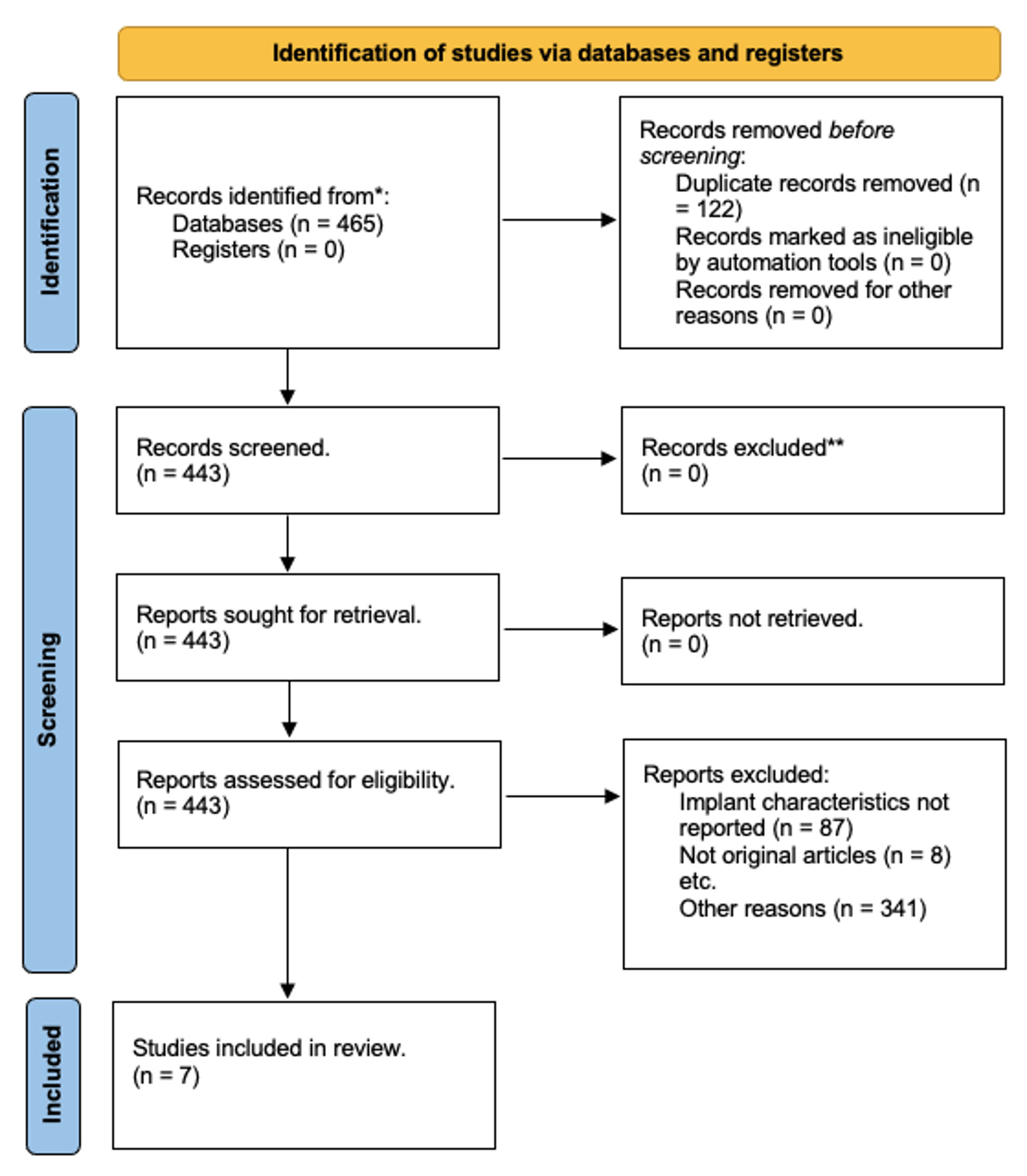
The focused question was built according to the PICO (Population, Intervention, Comparison, Outcome) scheme6. It answers the questions: “Who are the patients?—polyomyelitis patients” for “P” or population, “What are they exposed to?—TKA” for “I” or intervention, “What do we compare them to?—healthy controls undergoing TKA” for “C” or comparison and for “O” or outcome “What is the outcome?—the clinical outcomes”. A comprehensive search of PubMed, Medline, CINAHL, Cochrane, Embase, and Google Scholar databases was performed, covering the period between 1988 and 2022, and using various combinations of the following keywords: “total knee arthroplasty”, “tka”, “total knee replacement”, “tkr”, “poliomyelitis” and “polio”.
Two reviewers (FV and NDV) independently examined the titles and abstracts from all identified articles to assess their appropriateness to the research question. Full-text articles were ordered when required. In addition, each reference list from the identified articles was manually checked to verify that relevant articles were not missed. Case reports with lower than 2 patients were excluded. The quality of the included studies was assessed according to the level of evidence classification introduced by Wright et al7. Further, each study was evaluated for the following variables: study type, number of patients, radiographic preoperative deformities, and quadriceps muscular strength, type of prosthesis, follow-up period, clinical subjective and objective outcomes, and complications. Relevant data from each included study were extracted, recorded and are reported in Table 1 and Table 2.
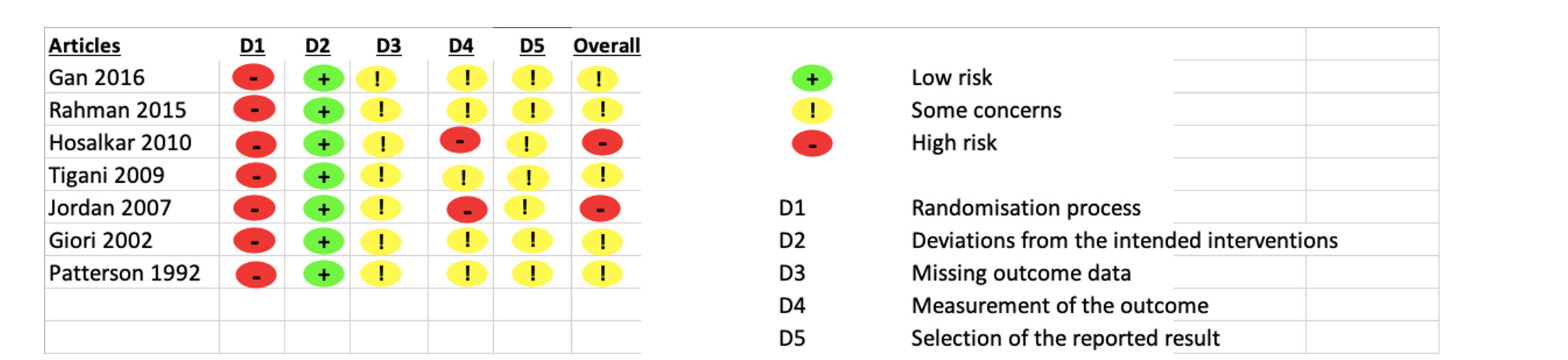
To assess the methodological quality of the included studies the Cochrane risk of bias in randomized trials (RoB 2)8 was employed.
Table 1. Patients preoperative characteristics and implants type.
| Authors and year of publication | Study Design | Knees (Patients) | Age
Sex |
Quadric. muscular strength* | Deformity | Type of prosthesis |
| Gan et al1,
2016 |
Retrospective
2002-2014 |
16 (14) | 62
NA |
3< – 2 PS, 1 CR
13=> – 2 CC, 6 PS, 8 CR |
10 varus (8°), 6 valgus (8.2°);
2 recurvatum (5-10°) and 10 flex deformity (12.8°) |
6 CR – 3 CS – 5 PS
2 CC (3 excl. for F-up<24 m) |
| Rahman et al8,
2015 |
Retrospective
1996-2013 |
14 (13) | 66
3M:10F |
5< 5 RH
9=> 9 RH |
Mean recurvatum=16.7° (10-30°) | RHK system “SMILES” with 5° of hypertext built-in
(stems were customized based on skeletal deformity) |
| Hosalkar et al9,
2010 |
Retrospective
1991-2005 |
10 | 66.5
3M:7F |
1< PS
3= 3 PS 6> 6 PS |
5 valgus (32°), 1 varus (20°),
3 recurvatum (10, 25, 50°) and a 10° flex contracture |
PS
(minimize stress on osteoporotic bone) |
| Tigani et al12,
2009 |
Retrospective
2000-2008 |
10 | 59
2M:8F |
4< – 3 RH, 1 CC
5= – 4 RH, 1 CC 1> – PS |
8 varus avg 15,4° (3-23°), 2 valgus (8 and 20°),
4 recurvatum 18° (5-35°) Patellar ratio=0.61 |
1 PS
2 CC 7 RH (3° hypertext.) for all < GMS |
| Jordan et al10,
2007 |
Retrospective 1991-2001 | 17 (15) | 62
3M:12F |
2< – 1 RH, 1PS
2= – 1CC, 1PS 13> – 7CC, 6PS |
1 recurvatum of 8°,
8 flex deformity of 9° (5-15°), 16 valgus avg 16.7° (4-28°) |
8 PS
8 CC 1 RH |
| Giori et al4,
2002 |
Retrospective
1970-2000 |
16 | 65
NA |
3< – 1 CC, 2 CR
3= – 1 CC, 2 CR 10> – 2 CC, 6 PS, 2 CR |
8 recurvatum avg 14° (5-30°), 2 flex of 15°,
11 valgus avg 18.8°; 2 varus (4° and 5°) 11 ML instab, 9 AP instab; 11 patella baja |
6 CR
6 PS 4 CC |
| Patterson et al11, 1992 | Retrospective
1974-1990 |
9 | 68
2M:7F |
3< – 1 CC, 2 PS
2= – 1 CC, 1 PS 4> – 1 RH*, 2 CC*, 1 PS* |
2 recurvatum
2 recurvatum and valgus 2 varus and 1 valgus |
4 PS
4 CC 1 RH |
RH: Rotating Hinged; PS: Posterior Stabilized; CR: Cruciate Retaining; CS: Cruciate Substituting; CC: Condylar Constrained; GMS: Gravity Muscle Strength; KAFO: Knee-Ankle-Foot Orthesis. *Muscular strength compared to antigravity.
Statistical Analysis
All the analyses were performed using STATA v.17 (StataCorp., TX, USA). Descriptive statistics were calculated. The Shapiro-Wilk test was employed to assess the dataset, and a normal distribution of the data was observed. Therefore, the Student’s t-test with two tails test for paired sample was used to compare the preoperative and postoperative values of KSS. The p<0.05 was considered significant.
Table 2. Outcomes and complications.
| Authors and year of publication | Follow-up | Complications | Preop KSS | Postop KSS | Results |
| Gan et al1,
2016 |
44 m | 1 valgus deformity 30° at 42 month follow-up (PS);
1 recurvatum (CR); 1 revision for loosening (CC); 1 MUA (RH) |
Knee 26.9
Pain 2.5 Function 40.6 |
82.3*
46.6* 61.6 (p<0.02) |
AKS score improved in all patients. OKS improved 40.9->20.8*; SF36 Pain=22.6->72.1*; Funct=25->56.6* No correlation of quad. strength with an increased risk of hypertext. There may be an increased risk of complications (stiffness and hypertext.) in relatively young patients (<60 y). *p<0.001. |
| Rahman et al8,
2015 |
72 m | 1 periprosthetic fracture of the tibia (RH);
1 MUA (RH) |
N/A | N/A | OKS: 10.6->30.7 (p<0.001). Mean recurvatum was 16.7° and decreased postop to 1.4°. 9/10 patients were satisfied or very satisfied. |
| Hosalkar et al9,
2010 |
92 m | Distal femoral shaft fracture treated nonoperatively (PS) | KSS 28 | 88* | Authors stressed the importance of the orthotic care, all patients wore a KAFO postop, those with quad. weakness required it lifetime. ROM=70->105°. Pain: 7->0.7. Ambulatory function: 2.9-> 4.5. |
| Tigani et al12,
2009 |
59 m | 1 infection (RH);
1 recurvatum (CC, 35° preop recurvatum) |
Knee 37
Function 38.5 |
75.7
54.3 |
77% of good or excellent results. Functional only 22% of good results. |
| Jordan et al10,
2007 |
42 m
(24-88) |
1 DVT (PS); 2 MUA (CC-RH); 1 mild ML instability (PS); 1 flexion contracture of 5°; 3 nonprogressive radiolucent line |
33
Pain 20.5 Stability 9.5 Function 27 |
85
48.5 23 37.6 |
All patients improved functional and pain scores. (no patients <70); Motion remain almost unchanged: 103.5 -> 107.5°.
No correlation between quad weakness and final outcome. |
| Giori et al4,
2002 |
71 m | 4 instabilities (2CR-1PS-1CC);
2 periprosthetic fractures (CR-PS); 1 transient peroneal nerve palsy (PS); 1 patellar tendon avulsion (CR) |
Knee 32.9
Pain 19.1 Function 28.6 |
73.3
40.5 34 |
The severity of preop laxity and deformity was associated with the severity of quad involvement. KSKS improved for all patients with quadriceps > GMS, but there was less pain relief in patients with quadriceps <GMS. ROM -5/110 -> -15/94. Postoperative instability and functional deterioration weren’t associated to muscular strength. |
| Patterson et al11, 1992 | 82 m | 3 revisions:
1 infection (CC) 2 instability (CC) |
Knee
Function |
84
25 |
TKA relieves pain, but functional outcome is poor.
HSS=70. 3 patients confined to wheelchairs. Recurrent deformities are probably due to the use of unconstrained device |
RH: Rotating Hinged; PS: Posterior Stabilized; CR: Cruciate Retaining; CS: Cruciate Substituting; CC: Condylar Constrained; KSS: Knee Society Score: Knee /100 (Pain/50; Stability/25); Function/100; OKS: Oxford Knee Score/60; HSS: Hospital for Special Surgery rating scale; DVT: deep vein thrombosis; Manipulation Under Anesthesia.
Results
A total of 7 studies1,4,8-12 published between 1988 and 2022 that reported total knee arthroplasty outcome in patients with poliomyelitis were finally included in the review (Table 1).
Level of Evidence
No controlled studies were available in the literature. All the papers were case series (Level of Evidence IV).
Patients
Seven studies1,4,8-12 were included in the review involving 87 patients with poliomyelitis undergone primary total knee arthroplasty on an affected limb (Table 1). A total of 92 knees (87 patients) were treated with arthroplasty. The gender of the patients was available in all studies, except two4,9, with a total of 13 males, 44 females and 30 patients whose sex was not reported. The age at surgery was recorded in all studies, with an overall mean of 63.9 years (Table 3).
Table 3. Data extracted from included studies.
| Number of knees (patients) | 92 (87) | ||
| Mean age at surgery (months) | 63.9 | ||
| Sex | Male | 13 | 15% |
| Female | 44 | 51% | |
| Not reported | 30 | 34% | |
| Deformities avg and number |
Recurvatum | 33 | 15.9 |
| Flex | 19 | 11.1 | |
| Valgus | 40 | 17.8 | |
| Varus | 23 | 11 | |
| Quadriceps muscular strength | Less than GMS | 21 | 23% |
| Equal to GMS | 15 | 16% | |
| Equal/More | 22 | 24% | |
| More than GMS | 34 | 37% | |
| Type of implant | CR | 12 | 13% |
| CS | 3 | 3% | |
| PS | 34 | 37% | |
| Unconstrained (CR+CS+PS) | 49 | 53% | |
| Constrained (CC) | 20 | 22% | |
| Rotating Hinged (RH) | 23 | 25% | |
| Mean follow-up | 66 months | ||
| Complications | Recurrent deformity/instability (3 CR, 3 PS, 4 CC, 1 N/A) | 11 | 12% |
| MUA (3 RH, 1 CC) | 4 | 4% | |
| PPFractures (1 CR, 2 PS, 1 RH) | 4 | 4% | |
| Infection (1 CC,1 RH) | 2 | 2% | |
| Loosening (CC) | 1 | 1% | |
| Others* | 3 | 3% | |
| KSS | KSS pain preop | 13.5 | |
| KSS pain postop | 45.7 | ||
| KSS knee preop | 31.3 | ||
| KSS knee postop | 80.8 | ||
| KSS function preop | 34.1 | ||
| KSS function postop | 43.7 | ||
*Transient peroneal nerve pulsy, patellar tendon avulsion and DVT.
Knee axial deformities were collected for all patients (Table 1). On the sagittal plane, 33 knees presented a recurvatum deformity with an average of 15,9° hyperextension, whereas 19 knees had the opposite deformity with an average of 11.1° flexion contracture. On the frontal plane, 40 knees presented a valgus deformity (mean 17.8°), while 23 were varus (mean of 11°).
All studies reported the preoperative quadriceps strength. Four studies6,8,9,13 measured quadriceps strength from 0 to 5, according to the Medical Research Council (MRC) manual muscle testing grading systems13. Other authors classified the muscular strength based on whether it was greater than, equal to, or lower than antigravity (Table 4)4,9. To sum up, 21 patients had a quadriceps muscular strength (QMS) lower than antigravity (0-2/5); 15 patients had a QMS equal to antigravity (3/5); 22 patients had a QMS equal or greater than antigravity; 33 patients had a QMS greater than antigravity (4-5/5) (Table 1).
Table 4. Clinical muscular weakness classification.
| Medical Research Council (MRC)
manual muscle testing grading systems13 |
Muscular strength compared to antigravity | |
| No contraction, paralysis | 0 | Less than antigravity (<) |
| Trace of contraction | 1 | |
| Moves if gravity is eliminated | 2 | |
| Moves against gravity | 3 | Equal to antigravity (=) |
| Moves against gravity and some resistant | 4 | Greater than antigravity (>) |
| Normal strength | 5 | |
Surgical Reports
Prostheses of varying designs and different levels of constraint were used by the authors. Of 92 TKA, 23 were rotating hinged (RH) implants, 20 were constrained and the remaining 49 were unconstrained. Among the unconstrained, 34 were posterior stabilized (PS), 12 were cruciate-retaining (CR) and 3 cruciate substituting (CS). Concerning the choice of implant, one author1 reported a transition from CR to more constrained implants after noticing knee instability in the initial cases.
Rehabilitation
Among the 7 articles included, only 3 of them1,4,9 clearly explained the rehabilitative protocol. In one article1, no braces were used and the standard institution physiotherapy was started. In another study4, two knees with quadriceps strength lower than or equal to antigravity were braced. In the third study9, all patients underwent extensive rehabilitation and a knee-ankle-foot orthosis was placed on all knees postoperatively.
Reported Outcomes
The mean follow-up was 66 months (range 42-92). Clinical and functional outcomes were evaluated using the KSS, OKS, SF 36 and the ROM difference, quadriceps strength. The clinical outcomes were evaluated using the Knee Society Score (KSS) in all studies, with the exception of one study8. In all abovementioned studies all the 3 parameters of the KSS (pain, knee and function) were available, both preoperatively and postoperatively, except for one study11 for which only the postoperative pain and function score were reported, and another study12 for which the preoperative and postoperative pain score was not reported. The postoperative mean KSS pain and knee score increased (corresponding to a reduction in pain) in all studies, from a mean of 13.5 (SD = 8.3) to 45.7 points (SD = 13.5) and the difference was statistically significant (p-value < 0.001), while the postoperative mean KSS function improved in all studies except for one study14, from a mean of 34.1 (SD = 11.4) to 43.7 points (SD = 8.5), and the difference was statistically significant (p-value < 0.001). Oxford Knee Score (OKS) was reported only in 2 studies1,8. In both studies, the OKS improved in all patients. The short form 36 health survey (SF-36) was reported only by one study1 and was shown to improve. The preoperative and postoperative Range of Motion (ROM) for flexion and extension of the knee were reported only in 2 studies1,4. The quadriceps muscle strength (QMS) and the degree of correction after surgery are described in detail in Table 1.
Complications
Out of 92 procedures, instability occurred seven times4,10,11 (four in unconstrained prostheses4,10 and three in constrained prostheses4,11); recurrent deformity occurred in three cases: recurvatum occurred two times (one in an unconstrained prosthesis1 and one in a constrained prosthesis12); valgus deformity occurred onw time1 (in an unconstrained prosthesis); overall two cases of infections were reported (one in a constrained prosthesis11 and one in a rotating hinged prosthesis12); a manipulation under anesthesia (MUA) was requested four times (three in rotating hinged prostheses8,10 and one in a constrained prosthesis10); periprosthetic fractures occurred four times (three in unconstrained prosthesis4,9 and one in rotating hinged prosthesis8); revision was performed four times, in one cases due to loosening1 (in constrained prosthesis), in one case due to infection11 (in a constrained prosthesis) and in two cases due to instability11 (in constrained prosthesis); patellar tendon avulsion occurred one time4 (in an unconstrained prosthesis); transient peroneal nerve palsy occurred one time4 (in an unconstrained prosthesis); deep vein thrombosis (DVT) occurred one time10 (in an unconstrained prosthesis).
Discussion
First of all, the main finding of this paper is the exiguity of literature available on this topic. This lack of literature is surely due to the rarity of this condition and the small number of surgeons able to perform such a challenging surgery.
Regarding this review, it has to be pointed out that the inclusion criteria were very flexible to reach the largest number of papers on the topic. A small sample size, different implants’ level of constraint, and the low quality of the outcome assessment were not considered exclusion criteria. The low quality of the included studies can be assessed in Figure 2, where the RoB 2 showed how two studies had high risk of bias9,10 and five moderate risk of bias1,4,8,11,12. However, only 7 studies were included in this review and they presented heterogeneity in terms of patients’ characteristics, type of prosthesis and rehabilitation protocols. Therefore, outcomes and complications were hardly comparable.
Figure 2. Methodological quality of the included studies the Cochrane risk of bias in randomized trials (RoB 2).
Deformities in the included studies were highly variable. The most frequently reported deformities were valgus and recurvatum knee, with some patients reaching 50° of axial deviation. The biomechanics of the lower limb was completely distorted and force distribution was grossly altered. Moreover, bone quality was often poor and all these factors were contrasting arguments in the choice of the type of implant and the level of constraint. Different types of prostheses were used in the included articles. The choice was based on different approaches to the problems to deal with. Hosalkar et al9 chose an unconstrained PS TKA for all patients without stems in order to minimize stress on osteoporotic bone. They reported good outcomes apparently without instabilities or recurrent deformities. However, all patients wore a Knee Ankle Foot Orthosis (KAFO) postoperatively, and those with quadriceps weakness required it lifetime.
Even though recurvatum is an alarming deformity, a mild degree of hyperextension confers stability to the knee because of an anatomic self-locking mechanism14. This stability is imperative for walking, especially with an impaired quadriceps muscular strength. A crucial issue is the choice of the level of constraint. Hinged implants12 provide intrinsic stability preventing the recurrence of laxity and deformities, notably recurvatum, in patients with poor muscle strength. This property meets the need for a higher degree of stability in the knee of the poliomyelitic patient, which is per se characterized by ligament laxity, axial and rotational deviation, poor bone quality and reduced muscular strength. This aspect has been noticed by two authors1,4 who reported a switch to more constrained implants after noticing failures with CR implants in their first cases. In addition to that, modern rotating hinge prosthesis allows more physiological kinematics by a better distribution of the sharing forces through the condyles rather than to the hinge mechanism12. The authors of the present paper strongly suggest the use of a rotating hinged implant providing intrinsic stability, thus preventing the need to wear orthosis to stabilize the knee. Otherwise, patients will have undergone an arthroplasty without having addressed the main problem of the joint and the cause of the osteoarthritis.
Indeed, choosing a rotating hinged implant does not only address the issue of improving clinical and functional outcomes, but also aims at targeting the main underlying pathologic process that led to the development of osteoarthritis, namely the instability. Thus, by acting at the root cause of the disease, the clinical sequelae derived from the persistence of the knee instability after primary total knee arthroplasty may be prevented. The choice of more constrained implants for this kind of patients, despite being probably a valid solution, is burdened by a high risk of failure due the intense mechanical stresses.
If on one hand stiff knee requiring Manipulation Under Anesthesia were reported only in constrained and hinged implants8,10, on the other hand, authors who preferred unconstrained prosthesis1,4,9 frequently reported instability and recurrent deformities, in particular, valgus and recurvatum deformity. Therefore, this type of prosthesis must be considered as a valid choice for primary TKA in patients affected by poliomyelitis, especially in the presence of lower antigravity quadriceps strength.
Limitations
The limits of this review are definitely the exiguous number of papers, the limited sample size and the poor level of evidence of such retrospective studies. Another major limitation is the lack of homogeneity in the patient population and the variability in the surgical approach, notably in the choice of implants. The combination of these two weaknesses made it impossible to compare outcomes and complications between different levels of constrained prosthesis and to find statistically significant differences or to identify with a reasonable degree of evidence which patients’ features can be considered as an indication for a specific type of prosthesis.
Conclusions
There are relatively few patients with poliomyelitis who have undergone TKA, limiting the number of studies available in literature. Such sample sizes are not sufficient for statistically meaningful subgroup analysis. However, good pain relief and functional outcome have been reported by several authors.
Ethics Approval
The following study was approved by the Institutional Review Board (Humanitas Ethical Committee) on 01/02/2022.
Conflicts of Interest
All authors report no conflict of interest.
ORCID ID
Filippo Vandenbulcke: 0000-0002-4603-659X
Francesco Manlio Gambaro: 0000-0002-0691-0369
Nicolò Danilo Vitale: NA
Francesco Iacono: 0000-0001-6825-2851
Maurilio Marcacci: 0000-0002-7484-1246
Tommaso Bonanzinga: 0000-0003-2861-4699
Funding
The current work has received no funding.
Data Availability
The uploading of the database of the current study on an online repository (Zenodo) is currently in progress.
Informed Consent
Not applicable.
References
- Gan ZJ, Pang HN. Outcomes of Total Knee Arthroplasty in Patients With Poliomyelitis. J Arthroplasty 2016; 31: 2508-2513.
- Pomeroy E, Fenelon C, Murphy EP, Staunton PF, Rowan FE, Cleary MS. A Systematic Review of Total Knee Arthroplasty in Neurologic Conditions: Survivorship, Complications, and Surgical Considerations. J Arthroplasty 2020; 35: 3383-3392.
- Prasad A, Donovan R, Ramachandran M, Dawson-Bowling S, Millington S, Bhumbra R, Achan P, Hanna SA. Outcome of total knee arthroplasty in patients with poliomyelitis. EFORT Open Rev 2018; 3: 358-362.
- Giori NJ, Lewallen DG. Total Knee Arthroplasty in Limbs Affected by Poliomyelitis. J Bone Joint Surg Am 2002; 84: 1157-1161.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4: 1.
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet 1999; 354: 1896-1900.
- Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am 2003; 85: 1-3.
- Rahman J, Hanna SA, Kayani B, Miles J, Pollock RC, Skinner JA, Briggs TW, Carrington RW. Custom rotating hinge total knee arthroplasty in patients with poliomyelitis affected limbs. Int Orthop 2015; 39: 833-838.
- Hosalkar HS, Fuller DA, Rendon N, Esquenazi A, Keenan MAE. Outcomes of total joint arthroplasties in adults with post-polio syndrome: results from a tertiary neuro-orthopaedic center. Curr Orthop Pract 2010; 21: 273.
- Jordan L, Kligman M, Sculco TP. Total knee arthroplasty in patients with poliomyelitis. J Arthroplasty 2007; 22: 543-548.
- Patterson BM, Insall JN. Surgical management of gonarthrosis in patients with poliomyelitis. J Arthroplasty 1992; 7: 419-426.
- Tigani D, Fosco M, Amendola L, Boriani L. Total knee arthroplasty in patients with poliomyelitis. Knee 2009; 16: 501-506.
- Vanhoutte EK, Faber CG, van Nes SI, Jacobs BC, van Doorn PA, van Koningsveld R, Cornblath DR, van der Kooi AJ, Cats EA, van den Berg LH, Notermans NC, van der Pol WL, Hermans MC, van der Beek NA, Gorson KC, Eurelings M, Engelsman J, Boot H, Meijer RJ, Lauria G, Tennant A, Merkies IS; PeriNomS Study Group. Modifying the Medical Research Council grading system through Rasch analyses. Brain 2012; 135: 1639-1649.
- Men HX, Bian CH, Yang CD, Zhang ZL, Wu CC, Pang BY. Surgical treatment of the flail knee after poliomyelitis. J Bone Joint Surg Br 1991; 73: 195-199.
To cite this article
What level of constraint for total knee arthroplasty in patients with poliomyelitis: a systematic review
JOINTS 2023;
1: e632
DOI: 10.26355/joints_20236_632
Publication History
Submission date: 06 Mar 2023
Revised on: 24 Apr 2023
Accepted on: 06 Jun 2023
Published online: 21 Jun 2023