JOINTS 2023;
1: e676
DOI: 10.26355/joints_20239_676
Magnetic resonance imaging evaluation of anterolateral ligament injuries and associated lesions in acute anterior cruciate ligament tears
Topic: Knee
Category: Original article
Abstract
OBJECTIVE: The first aim of our study was to investigate the appearance of the injured Anterolateral Ligament (ALL) on magnetic resonance imaging (MRI) performed in acute anterior cruciate ligament (ACL) injuries and provide data about the inter- and intra-rater agreement in assessing the ALL status. The second aim was to describe the incidence of associated injuries in acute ACL-injured knees and provide data regarding the inter- and intra-rater agreement in identifying these.PATIENTS AND METHODS: Patients with ACL lesions who underwent MRI within 10 days from the injury were included. Images were evaluated by an orthopedic surgeon and a musculoskeletal (MSK) radiologist. Inter- and intra-observer reliabilities were determined for MRI parameters of the anterolateral ligament (ALL) and associated injuries by using the kappa (κ) test.
RESULTS: A total of 100 patients were evaluated. ALL abnormalities were observed in 93% of the cases. Inter-observer reliability was substantial to almost perfect concerning ALL signal, femoral and tibial bone bruises, femoral notch sign and meniscal tears (κ = 0.6-1); moderate agreement was observed for lateral meniscus tears (κ = 0.56) and Segond fractures (κ = 0.45). Intra-observer reliability of the orthopedic surgeon was substantial to almost perfect for all the criteria evaluated (κ = 0.6-1). Intra-observer reliability of the MSK radiologist was substantial to almost perfect for ALL injuries and bone bruises (κ = 0.6-1); there was a moderate agreement for meniscal tears and Segond fractures (κ = 0.41-0.6), except for Lateral Meniscus Posterior Horn Root Tears (κ = 0.21).
CONCLUSIONS: MRI can represent an instrument of high reliability and reproducibility in the diagnosis of ALL tears and associated lesions in patients with acute ACL ruptures.
Introduction
The anterolateral ligament (ALL) has recently received renewed interest after its detailed anatomical description by Claes et al1 in 2013. Numerous studies1-3 have described its anatomy and the biomechanical role as an anterolateral knee stabilizer. Anatomical studies4-8 have shown the ALL origin posterior and proximal to the lateral epicondyle, a meniscal insertion between its anterior horn and body and a tibial insertion on the anterolateral edge of the tibia between Gerdy’s tubercle and the tip of the fibular head, around 5-10 mm below the lateral plateau.
Several biomechanical and clinical studies9-12 have recently shown that the ALL plays a role as a stabilizer of internal rotation. Moreover, other studies12,13 have found a high incidence of ALL lesions concomitant with anterior cruciate ligament tears and suggested that injuries to the ALL can result in residual anterolateral rotatory instability and poor outcomes, if not addressed at the time of ACL reconstruction (ACLR). For this reason, many authors14,15 have recently suggested indications for ALL reconstruction or lateral extra-articular tenodesis (LET) in cases of high-grade pivot shift, associated Segond fracture, chronic ACL lesions, high level of sporting activity, patients involved in pivoting sports, lateral femoral notch sign (FNS), young age females and ACL revisions.
Imaging studies4,6,8,16-18 for ALL assessment to allow a more precise preoperative planning are also growing in interest. Numerous studies in literature have also recently evaluated the efficacy of magnetic resonance imaging (MRI) and ultrasound (US) to characterize the ALL in both healthy and injured knees with conflicting results.
One of the primary concerns in the diagnosis of ALL lesions is the efficacy of MRI, with a percentage of identification ranging from 10% to 90%8,19-25. However, MRI is routinely used to assess other injuries associated with the ACL, particularly bone bruises, meniscal tears, chondral tears and the FNS. All these abnormalities are consequences of the injury mechanism that leads to an ACL tear, which is usually a rotation and translation phenomenon similar to the pivot shift (pivot shift-like injury)26,27.
Thus, the main objective of this study was to investigate the appearance of the injured ALL on MRI performed a maximum of 10 days after ACL injury and to provide data about the interrater agreement in assessing this ligament status. The second aim was to describe the MRI incidence of associated ALL injuries (FNS, bone bruises, meniscal and chondral tears) in acute ACL-injured knees and provide data regarding the interrater agreement in identifying and categorizing these injuries.
Patients and Methods
Patient Population
All subjects provided written informed consent for inclusion before they participated in the study. A retrospective analysis of prospectively collected data for consecutive patients who were admitted with a history of acute knee trauma from January 2018 to October 2018 at S. Andrea Hospital in Rome, was performed. Patients who were diagnosed with acute ACL injury were included in the study. Exclusion criteria: patients who sustained concomitant fractures (with the exception of Segond fractures) or had multiligamentous injuries that required surgery in addition to ACLR; patients with a history of previous surgery on the examined knee, or knee osteoarthritis.
MRI Assessment
All MRIs were performed within 10 days of the trauma. The MRI examinations were all performed with 1.5-mm slice thickness in the supine position on a 1.5 T system (Aera, Espree, or Avanto; Siemens Medical Solutions, Erlangen, Germany). The analysis was performed on a picture archiving and communication system workstation (Centricity RA 1000, GE Healthcare, Chicago, IL, USA). An orthopaedic surgeon and a musculoskeletal radiologist assessed the examinations twice with an interval of at least 2 weeks, in a randomized order and blinded from the readings of the other reader.
Before starting the study, the examiners reviewed 15 MRI scans to agree on the appearance of the ALL, its injuries and the classifications of the associated articular lesions.
According to Monaco et al28, the ALL was evaluated on coronal images, with the axial and sagittal planes used for anatomic orientation. The regular ALL was defined as the low signal band originating from the posterior-proximal region of the lateral epicondyle of the femur and crossing the proximal surface of the lateral collateral ligament, deep to the iliotibial band (ITB), to its tibial insertion between the Gerdy tubercle and the fibular apex. By T2-weighted scans, the readers assessed the ALL’s signal (regular or increased), thickness (regular or increased), fibers appearance (continuous or interrupted) (Figure 1), Segond fractures, and inferior lateral genicular artery (ILGA) appearance (Figure 2).
Figure 1. Anterolateral Ligament tear: Coronal T2 weighted MRI. The circle indicates abnormality of the inferior lateral genicular vessels (usually 2 circular areas of hyperintensity).
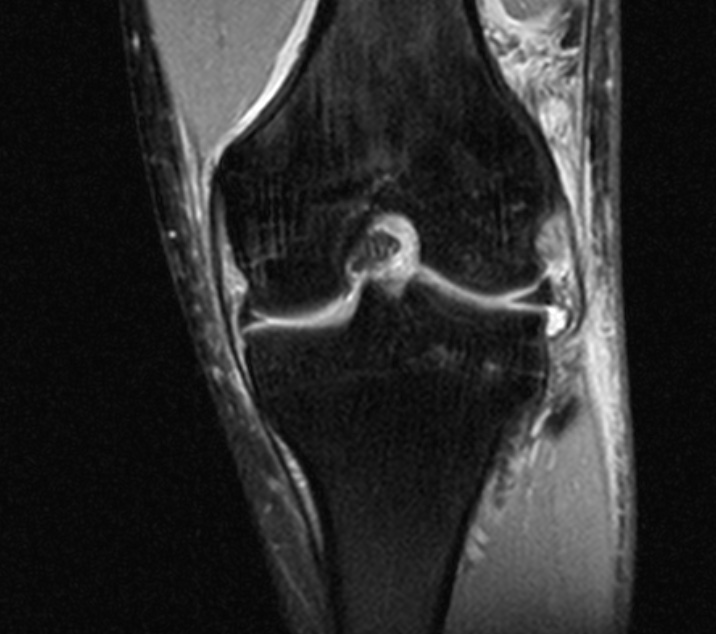
Figure 2. Asymmetry of the Genicular vessels: Coronal T2 weighted MRI. The circle indicates abnormality of the inferior lateral genicular vessels (usually 2 circular areas of hyperintensity).

The asymmetry of the genicular vessels was considered when a single circular finding was present (usually 2 circular areas of hyperintensity are observed, corresponding to the two vessels) or when the disappearance of one or both of the corresponding areas was observed29. Segond fracture was detected as a signal hyperintensity at tibial ALL’s insertion or hypointense partial detachment (Figure 3)30. Furthermore, associated lesions were evaluated. The bone contusions were defined as absent (none/minimal) or present (moderate or severe)31, and their location was assessed (medial/lateral tibial plateau, medial/lateral femoral condyle). The presence of FNS was detected on sagittal MRI images, highlighted as a depression greater than 2 mm or a low signal sulcus of the surface of the femoral condyle, an indicator of an osteochondral lesion (Figure 4).
Figure 3. Segond fracture: Coronal T2 weighted MRI. The circle indicates the Segond Fracture.

Figure 4. Femoral Notch Sign: Sagittal T2 weighted MRI. The circle indicates a depression suggestive for the Femoral Notch Sign.

Eventually, meniscal tears, particularly lateral meniscus posterior horn radial tears (LMPHRT) and medial meniscus posterior horn-capsular (Ramp) lesions were detected.
The Ramp lesions are better detectable on FAT-SAT T2-weighted sagittal scans32. A hyperintense streak or crack of effusion between the posterior horn of the medial meniscus and the capsular margin, an alteration of the signal at the periphery of the posterior horn and a bone-bruise of the posterior medial tibial plateau can be seen (Figure 5).
Figure 5. RAMP lesion: Sagittal T2 weighted MRI. The circle indicates the Ramp Lesion with an effusion between the posterior horn of the medial meniscus and the capsular margin.

The LMPHRTs were highlighted on T2-weighted and FAT-SAT T2-weighted sequences on the coronal and sagittal planes33. LMPHRT and root were identified, according to Asai et al34, thanks to the presence of two signs: the cleft sign (a vertical linear defect between the lateral femoral condyle and the intercondylar eminence on the coronal images), and the truncated triangle sign (an abrupt interruption of the regular triangular meniscal contour at its apex on the sagittal T2 images) (Figure 6).
Figure 6. Lateral meniscus posterior horn root tear: T2 weighted MRIs. a, Coronal, the circle indicates the Cleft Sign with a vertical linear defect between the lateral femoral condyle and the intercondylar eminence. b, Sagittal, the circle indicates the Truncated Triangle Sign, as an abrupt interruption of the regular triangular meniscal contour at its apex.

Statistical Analysis
The scoring results for all observers were calculated using SPSS Statistics for MacOS v. 25 (IBM Corp., Armonk, NY, USA). Cohen’s kappa coefficient was used to determine the degree of intra-observer and inter-observer agreement.
The kappa values were interpreted according to Landis and Koch35, i.e., κ < 0.00 corresponds to poor agreement, κ = 0.00-0.20 to a slight agreement, κ = 0.21-0.40 to fair agreement, κ = 0.41-0.60 to moderate agreement, κ = 0.61-0.80 to substantial agreement, and κ = 0.81-1.00 to almost perfect agreement.
The lesions were dichotomized to construct 2 – 2 tables to facilitate calculations. The inter-observer value was calculated in the second examination series. No adjustment for multiple testing was made.
Results
One hundred patients were eligible for inclusion in this study. The selected patients had a mean age of 28.3 ± 9.8 (mean ± SD) years. There were 74 males (74%) and 26 females (26%). The demographic data of the study groups are displayed in Table 1. The left side was affected in 60% of cases (60 patients) and the right side in 40% (40 patients). The observers’ mean records are displayed in Table 2. ALL abnormalities were found in 93% of MRIs; the most frequent were signal changes, found in 91% of cases; thickness variations were found in 69% of cases; fiber injuries in 39% of cases; ILGA abnormalities in 43% of cases. It can be observed that the most frequently encountered lesions were the femoral and tibial bone bruises (in 90% and 93% of the cases, respectively).
Table 1. Demographic data of patients.
| Total | |||
| Age | n | 100 | |
| Mean (SD) | 28.3 (9.8) | ||
| Median (Q1; Q3) | 27 (21; 33) | ||
| Min; Max | 13; 68 | ||
|
Gender |
n |
100 |
|
| Female | 26 (26%) | ||
| Male | 74 (74%) | ||
Table 2. Prevalence of MRI injuries.
| Lesion type | Patients, n (%) |
| ALL | |
| Signal | 91 (91%) |
| Thickness | 69 (69%) |
| Fibers | 39 (39%) |
| ILGA | 43 (43%) |
| FNS | |
| Yes | 59 (59%) |
| No | 41 (41%) |
| Bone Bruise | |
| Femoral | 90 (90%) |
| Tibial | 93 (93%) |
| Meniscal Tear | |
| None | 29 (29%) |
| Yes | 71 (71%) |
| Isolated Medial Meniscus | 13 (13%) |
| Isolated Lateral Meniscus | 29 (29%) |
| Both | 29 (29%) |
| LMPHRT | |
| Yes | 41 (41%) |
| No | 59 (59%) |
| Ramp Lesion | |
| Yes | 35 (35%) |
| No | 65 (65%) |
| Segond Fracture | |
| Yes | 7 (7%) |
| No | 93 (93%) |
ALL, anterolateral ligament; FNS, femoral notch sign; ILGA, inferior lateral geniculate artery; LMPHRT, lateral meniscus posterior horn root tear.
Concerning intra-observer variability, a substantial agreement to an almost perfect agreement was noted for both observers: the first and second observers achieved mean κ-values of 0.84 and 0.67, respectively, ranging from substantial to almost perfect agreement.
An inter-observer agreement, demonstrated by κ-values, ranged from 0.45 for Segond fractures (fair agreement) to 0.86 for FNS (almost perfect agreement).
Assessment of the intra- and inter-observer agreements are represented in Table 3.
Table 3. Measurement of observers’ agreement.
| ALL | Bone Bruise | FNS | Meniscus | Segond | ||||||||
| Signal | Thickness | Fibers | ILGA | Femur | Tibia | MM | LM | LMPHRT | Ramp | |||
| Inter-observer κ | .8 | .72 | .65 | .64 | 1 | 1 | .86 | .77 | .56 | .61 | .84 | .45 |
| Inter-observer agreement rate, % | 94.7 | 86.4 | 78 | 73.6 | 100 | 100 | 90.6 | 89.2 | 70.8 | 75 | 93.7 | 55 |
| Intra-Observer 1 κ | .73 | .75 | .88 | .64 | 1 | 1 | .86 | .83 | .94 | .77 | .78 | .90 |
| Intra-Observer 1 agreement rate, % | 93.1 | 83.4 | 91.9 | 79.2 | 100 | 100 | 93.1 | 91.7 | 97.2 | 88.9 | 90.3 | 94.1 |
| Intra-Observer 2 κ | .8 | .77 | .88 | .66 | 1 | 1 | .58 | .57 | .42 | .21 | .57 | .58 |
| Intra-Observer 2 agreement rate, % | 86.1 | 79.4 | 93.3 | 75.6 | 100 | 100 | 75 | 68.1 | 67.2 | 52.5 | 79.2 | 76.1 |
Cohen’s κ values and agreement rates are expressed by comparing operator 1 to operator 2 (Inter-observer), operator 1 at the first measurement to operator 1 at the second measurement (Intra-observer 1), and operator 2 at the first measurement to operator 2 at the second measurement (Intra-observer 2). For Cohen’s κ, its value and statistical significance were calculated. Values which did not reach statistical significance (p<0.05) are shown in bold. The agreement rate is expressed as a percentage.
Discussion
The study found that the Anterolateral Ligament (ALL) was clearly visualized in MRI in most cases of acute Anterior Cruciate Ligament (ACL) ruptured knees with a high prevalence of injuries. Signal abnormalities were found in 91% of cases, thickness affected 69% of cases, fiber injuries were detected in 39%, and ILGA asymmetries in 43% of cases. Associated intraarticular lesions, such as meniscal tears, Ramp lesions, LMPHRT, bone bruising, and FNS were frequently found alongside ALL injuries. In this study, a high sensitivity of MRI was observed, identifying lesions of ALL in up to 91% of patients, with an excellent reproducibility confirmed by a high intra-observer (κ = 0.73-0.8) and inter-observer (κ = 0.8) agreement. For the other parameters, inter-observer agreement ranged from moderate (κ = 0.45) to almost perfect (κ = 1), and intra-observer agreement ranged from fair (κ = 0.21) to almost perfect (κ = 1).
To date, the diagnostic procedure in the event of an ACL rupture can no longer ignore the evaluation and identification of associated structures tears as those analyzed in the current paper, due to their biomechanical function. Impairment of these leads to increased anteroposterior and rotational instability, which probably cannot be corrected with an isolated ACL reconstruction15.
It is particularly important to systematically search for lesions of the ALL on MRI because of the clinical implications they may have. MRI ALL abnormalities in patients with ACL injuries have a significant association with pivot shift test results in patients under anesthesia36. At present, a remarkable variability can be seen in MRI in the identification rate of ALL lesions. Recently, Ferretti et al29 have used the MRI of the uninjured side as a comparison to detect ALL lesions in acutely ACL-injured knees; they found that, when using the healthy side as a comparison, the percentage of ALL injury is up to 88.2% with an inter- and intra-observer agreement ranging from 0.81 to 1. Cavaignac et al18, in an MRI study of 30 knees, found the tibial portion of the ALL to be injured in 100% of cases. The variability of protocols used for MRI scans, radiologic signs, and time from injury to MRI results in high variability of ALL lesions on MRI, ranging from 10.8% to 78.8%8,11,18,19,22,25,30,37-39. This study’s high prevalence of ALL abnormalities may be due to the acute setting in which the MRI was performed, prior to the reparative process involving ALL. In fact, it has been suggested40 that rates are lower in chronic ACL-injured knees, indicating that some ALL injuries heal. Saithna et al41, have recently explored the rate and duration of the healing process of ALL injuries following anterior cruciate ligament reconstruction ACLR using serial 3 T, 3D-MRI scans. Among the 44 patients in the study, 71.2% had preoperative ALL injuries. The authors found that 30.3% of ALL injuries fully healed by 12 months after ACLR, but none of the patients with a complete ALL tear was observed to achieve full healing. This study suggested that the healing process for ALL injuries after ACLR is generally slow, with only a small proportion of patients experiencing a full recovery.
An alteration of the ILGA was detected in 43% of cases, also with excellent inter-observer agreement (κ = 0.64), suggesting that this sign, if detected, could help in the diagnosis of ALL lesions. An overlapping variability is also evident in the identification of the Segond fractures. In multiple published studies19,42, its prevalence varies from 1.8% to more than 36% of injured ALL. Following these previous studies, avulsion fractures were found in 7% of the patients examined in this study, with a moderate inter-observer agreement (κ = 0.45).
Recently, many authors43-46 have tried to correlate and confirm a pivot-shift-like mechanism in ACL injuries with lesions found on MRI. Several papers have reported18,28,29,47 an association between lateral bone bruising and abnormalities of the ALL, supporting the hypothesis of a rotational injury mechanism that leads to an ACL and ALL tear. Helito et al48 found that only 1 out of 66 cases of ALL injury was not accompanied by a bone bruise, and that ALL injury was present for 46.5% of the time when both lateral femoral condyle (LFC) and lateral tibial plateau (LTP) bone bruises were present. Another study showed that 37.5% of acute ACL tears with LFC and LTP bone bruises were associated with an ALL injury8 . Similarly, Lintin et al49 found that 68 of 75 cases of ALL injury had an associated bone bruise. Their findings were supported by two studies by Lee et al31, who found an increased risk of ALL injury with the presence of bone bruises and an increased severity of ALL injury with the presence of bone bruise50. However, Marot et al51 found no correlation between ALL injury and bone bruise volume. In the present study, these results were confirmed with an elevated prevalence of BB both in the tibial plateau (93%) and in the femoral condyles (90%) with the same typical distribution on the sagittal plane in the lateral portions, in association with lesions of the lateral meniscus in 58% and with perfect interrater concordance (κ = 1).
The literature shows a high prevalence of lateral meniscus injuries associated with ACL rupture52. Many authors considered the Lateral Meniscus (LM) injury being correlated to the ALL insertion on it5,31,53. Helito et al7 and Caterine et al5, in their cadaveric studies, described the presence of an ALL-meniscal insertion. These authors assumed that meniscus could break due to the pulling of the ALL, during the pivot shift phenomenon. Meniscal ruptures, with particular reference to lesions of the posterior horn, may be caused to entrapment of the meniscus between the posterior aspect of the LTP and the LFC31,54.
LMPHRT had been commonly associated with anterior cruciate ligament injuries, with an incidence ranging from 4% to 52%55-57, probably caused by the rotational ACL injury mechanism45,58. Lee et al31, analyzing 275 MRI scans in patients with acute ACL rupture, found lesions of the external meniscus in 42% of the cases with ALL displayed, with a prevalence of these significantly higher in the case of injured ALL (p < 0.03); moreover, they reported a correlation of LMPHRT with ALL lesions (14.8% and 6.4% in injured and healthy ALL, respectively, p = 0.042). In the present study, we found, in agreement with Lee, a high prevalence of lateral meniscus lesions with an excellent inter-rater concordance (κ = 0.77-0.83). This remarkable datum is due to the fact that a distinction has not been made between root lesions and proper radial lesions when referring to lesions of the posterior horn of the lateral meniscus. Moreover, as we performed the MRIs in a very acute phase, the joint effusion could lead to an overestimation of the LMPHT.
In the present study, we also detected lesions of the medial meniscus in 42% of the cases, with excellent inter-rater concordance (κ = 0.86). Among these, we have found the Ramp lesions to be diagnosed by MRI in 35% of patients. Since Ramp lesions may remain hidden in the anterior (at 90° of flexion) or anterolateral “standard” arthroscopic approach, a preoperative suspicion for knee surgeons is needed to diagnose and treat these lesions59, and MRI could be a useful tool. DePhillipo et al60 detected an incidence of Ramp lesions in 16.6% of knees with ACL rupture and low sensitivity of MRI, able to identify these lesions in only 48% of the cases, compared to the gold-standard arthroscopic exploration. A significant result in our study, compared to the previous ones in literature, was a higher identification rate of Ramp lesions, resulting in 35% of injured knees, with an almost perfect inter/intra-observer concordance, demonstrated by kappa values of 0.84 and 0.78, respectively. This result should be explained because the MRIs were in the early phase after injury, and some alterations, such as an evident effusion and imbibition of the periarticular tissues due to the effusion, can be correlated to the recent injury and not only to the Ramp lesion.
Another typical lesion associated with ACL ruptures is the Lateral FNS, represented by the presence of a deep notch on the lateral femoral condyle. In the present study, we found a significantly higher percentage of the Lateral FNS compared in the previous literature, with an almost perfect inter-rater agreement (κ = 0.86). Although various studies61,62 had hypothesized that this diagnostic sign could result by chronic rotational instability, more precisely the anterior subluxation of the lateral tibial plateau, causing recurrent impacts on the lateral femoral condyle, we found it in the majority of the acute cases we studied. Other studies63 suggest that it may be the result of the progression of occult osteochondral lesions that occur because of traumatic valgus injuries at the time of ACL tearing, in part analogous to a Hill-Sachs injury during shoulder dislocations.
Limitations and Strengths
We are aware of possible limitations of the study as the injury criteria were established arbitrarily based on the experience of the authors and on previous studies in literature which evaluated these structures. Moreover, the number of patients is not high, and a power analysis was not performed, but the study population can be considered in line with similar studies31,48. Another limitation is represented by using a 1.5 T MRI, while other recent studies in literature have highlighted a higher accuracy of the 3T scans.
On the other hand, the main strength of our study is represented by having assessed the majority of the associated lesions in ACL rupture only in patients with an acute injury, so we provided a real estimation of the lesions associated with the first trauma, without confounding factors due to possible subsequent traumas or recurrent instability.
Conclusions
MRI can represent an instrument of high reliability and reproducibility in the diagnosis of lesions of the anterolateral ligament and associated lesions in patients with acute ACL rupture.
Ethics Approval
This study was conducted in accordance with the Declaration of Helsinki of 1975 (as revised in 2013), and the protocol was reviewed and approved by the Ethics Committee of the University of Rome La Sapienza (Ref. number: 5713_2018).
Informed Consent
All subjects provided written informed consent for inclusion before they participated in the study.
Conflict of Interest
Edoardo Monaco and Andrea Ferretti are Arthrex paid Consultants.
ORCID ID
Alessandro Carrozzo: 0000-0003-0700-8139
Funding
None.
Data Availability
Data are available on request.
References
- Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat 2013; 223: 321-328.
- Monaco E, Ferretti A, Labianca L, Maestri B, Speranza A, Kelly MJ, D’Arrigo C. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc 2012; 20: 870-877.
- Claes S, Luyckx T, Vereecke E, Bellemans J. The segond fracture: A bony injury of the anterolateral ligament of the knee. Arthroscopy 2014; 30: 1475-1482.
- Helito CP, Helito PVP, Costa HP, Bordalo-Rodrigues M, Pecora JR, Camanho GL, Demange MK. MRI evaluation of the anterolateral ligament of the knee: Assessment in routine 1.5-T scans. Skeletal Radiol 2014; 43: 1421-1427.
- Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A. A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc 2015; 23: 3186-3195.
- Porrino J, Maloney E, Richardson M, Mulcahy H, Ha A, Chew FS. The anterolateral ligament of the knee: MRI appearance, association with the segond fracture, and historical perspective. AJR Am J Roentgenol 2015; 204: 367-373.
- Helito CP, Bonadio MB, Soares TQ, da Mota e Albuquerque RF, Natalino RJ, Pécora JR, Camanho GL, Demange MK. The meniscal insertion of the knee anterolateral ligament. Surg Radiol Anat 2016; 38: 223-228.
- Helito CP, Helito PVP, Costa HP, Demange MK, Bordalo-Rodrigues M. Assessment of the Anterolateral Ligament of the Knee by Magnetic Resonance Imaging in Acute Injuries of the Anterior Cruciate Ligament. Arthroscopy 2017; 33: 140-146.
- Parsons EM, Gee AO, Spiekerman C, Cavanagh PR. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med 2015; 43: 669-674.
- Sonnery-Cottet B, Lutz C, Daggett M, Dalmay F, Freychet B, Niglis L, Imbert P. The Involvement of the Anterolateral Ligament in Rotational Control of the Knee. Am J Sports Med 2016; 44: 1209-1214.
- Song GY, Zhang H, Wu G, Zhang J, Liu X, Xue Z, Qian Y, Feng H. Patients with high-grade pivot-shift phenomenon are associated with higher prevalence of anterolateral ligament injury after acute anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 2017; 25: 1111-1116.
- Ferretti A, Monaco E, Gaj E, Andreozzi V, Annibaldi A, Carrozzo A, Vieira TD, Sonnery-Cottet B, Saithna A. Risk Factors for Grade 3 Pivot Shift in Knees With Acute Anterior Cruciate Ligament Injuries: A Comprehensive Evaluation of the Importance of Osseous and Soft Tissue Parameters From the SANTI Study Group. Am J Sports Med 2020; 48: 2408-2417.
- Puzzitiello RN, Agarwalla A, Zuke WA, Garcia GH, Forsythe B. Imaging Diagnosis of Injury to the Anterolateral Ligament in Patients With Anterior Cruciate Ligaments: Association of Anterolateral Ligament Injury With Other Types of Knee Pathology and Grade of Pivot-Shift Examination: A Systematic Review. Arthroscopy 2018; 34: 2728-2738.
- Helito CP, Bonadio MB, Gobbi RG, da Mota E Albuquerque RF, Pécora JR, Camanho GL, Demange MK. Combined Intra- and Extra-articular Reconstruction of the Anterior Cruciate Ligament: The Reconstruction of the Knee Anterolateral Ligament. Arthrosc Tech 2015; 4: e239-244.
- Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BHB, Murphy CG, Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med 2015; 43: 1598-1605.
- De Carli A, Monaco E, Mazza D, Argento G, Redler A, Proietti L, Gaj E, Ferretti A. Assessment of the anterolateral ligament of the knee by magnetic resonance imaging. Joints 2018; 6: 153-156.
- Taneja AK, Miranda FC, Braga CA, Gill CM, Hartmann LG, Santos DC, Rosemberg LA. MRI features of the anterolateral ligament of the knee. Skeletal Radiol 2015; 44: 403-410.
- Cavaignac E, Wytrykowski K, Reina N, Pailhé R, Murgier J, Faruch M, Chiron P. Ultrasonographic identification of the anterolateral ligament of the knee. Arthroscopy 2016; 32: 120-126.
- Claes S, Bartholomeeusen S, Bellemans J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg 2014; 80: 45-49.
- Helito CP, Helito PV, Bonadio MB, Pécora JR, Bordalo-Rodrigues M, Camanho GL, Demange MK. Correlation of Magnetic Resonance Imaging With Knee Anterolateral Ligament Anatomy: A Cadaveric Study. Orthop J Sports Med 2015; 3: 2325967115621024.
- Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M. Anterolateral Ligament Reconstruction Is Associated with Significantly Reduced ACL Graft Rupture Rates at a Minimum Follow-up of 2 Years: A Prospective Comparative Study of 502 Patients from the SANTI Study Group. Am J Sports Med 2017; 45: 1547-1557.
- Kızılgöz V, Sivrioğlu AK, Aydın H, Çetin T, Ulusoy GR. Assessment of the anterolateral ligament of the knee by 1.5 T magnetic resonance imaging. J Int Med Res 2018; 46: 1486-1495.
- Marshall T, Oak SR, Subhas N, Polster J, Winalski C, Spindler KP. Can the Anterolateral Ligament Be Reliably Identified in Anterior Cruciate Ligament–Intact and Anterior Cruciate Ligament–Injured Knees on 3-T Magnetic Resonance Imaging? Orthop J Sports Med 2018; 6: 2325967118796452.
- Andrade R, Rebelo-Marques A, Bastos R, Zaffagnini S, Seil R, Ayeni OR, Espregueira-Mendes J. Identification of Normal and Injured Anterolateral Ligaments of the Knee: A Systematic Review of Magnetic Resonance Imaging Studies. Arthroscopy 2019; 35: 1594-1613.
- Devitt BM, O’Sullivan R, Feller JA, Lash N, Porter TJ, Webster KE, Whitehead TS. MRI is not reliable in diagnosing of concomitant anterolateral ligament and anterior cruciate ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc 2017; 25: 1345-1351.
- Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: A systematic review. Sports Med 2014; 44: 281-293. https://pubmed.ncbi.nlm.nih.gov/24158783/
- Anderson MJ, Browning WM, Urband CE, Kluczynski MA, Bisson LJ. A Systematic Summary of Systematic Reviews on the Topic of the Anterior Cruciate Ligament. Orthop J Sports Med 2016; 4: 2325967116634074.
- Monaco E, Helito CP, Redler A, Argento G, De Carli A, Saithna A, Helito PVP, Ferretti A. Correlation Between Magnetic Resonance Imaging and Surgical Exploration of the Anterolateral Structures of the Acute Anterior Cruciate Ligament–Injured Knee. Am J Sports Med 2019; 47: 1186-1193.
- Ferretti A, Monaco E, Redler A, Argento G, De Carli A, Saithna A, Helito PVP, Helito CP. High Prevalence of Anterolateral Ligament Abnormalities on MRI in Knees With Acute Anterior Cruciate Ligament Injuries: A Case-Control Series From the SANTI Study Group. Orthop J Sports Med 2019; 7: 2325967119852916.
- Faruch Bilfeld M, Cavaignac E, Wytrykowski K, Constans O, Lapègue F, Chiavassa Gandois H, Larbi A, Sans N. Anterolateral ligament injuries in knees with an anterior cruciate ligament tear: Contribution of ultrasonography and MRI. Eur Radiol 2018; 28: 58-65.
- Lee DW, Lee JH, Kim JN, Moon SG, Kim NR, Kim DH, Kim JG. Evaluation of Anterolateral Ligament Injuries and Concomitant Lesions on Magnetic Resonance Imaging After Acute Anterior Cruciate Ligament Rupture. Arthroscopy 2018; 34: 2398-2406. https://pubmed.ncbi.nlm.nih.gov/29730210/
- DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF. Incidence and Detection of Meniscal Ramp Lesions on Magnetic Resonance Imaging in Patients With Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2017; 45: 2233-2237.
- Laundre BJ, Collins MS, Bond JR, Dahm DL, Stuart MJ, Mandrekar JN. MRI accuracy for tears of the posterior horn of the lateral meniscus in patients with acute anterior cruciate ligament injury and the clinical relevance of missed tears. AJR Am J Roentgenol 2009; 193: 515-523.
- Asai K, Nakase J, Oshima T, Shimozaki K, Toyooka K, Tsuchiya H. Lateral meniscus posterior root tear in anterior cruciate ligament injury can be detected using MRI-specific signs in combination but not individually. Knee Surg Sports Traumatol Arthrosc 2020; 28: 3094-3100.
- Landis JR, Koch GG. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977; 33: 159-174.
- Helito PVP, Helito CP, Rodrigues MB. Anterolateral ligament MRI of the knee in ACL injuries: MRI abnormalities association with instability. Eur Radiol 2022; 33: 1456-1464.
- McDonald LS, van der List JP, Jones KJ, Zuiderbaan HA, Nguyen JT, Potter HG, Pearle AD. Passive Anterior Tibial Subluxation in the Setting of Anterior Cruciate Ligament Injuries: A Comparative Analysis of Ligament-Deficient States. Am J Sports Med 2017; 45: 1537-1546.
- Hartigan DE, Carroll KW, Kosarek FJ, Piasecki DP, Fleischli JF, D’Alessandro DF. Visibility of Anterolateral Ligament Tears in Anterior Cruciate Ligament–Deficient Knees With Standard 1.5-Tesla Magnetic Resonance Imaging. Arthroscopy 2016; 32: 2061-2065.
- Kosy JD, Schranz PJ, Patel A, Anaspure R, Mandalia VI. The magnetic resonance imaging appearance of the anterolateral ligament of the knee in association with anterior cruciate rupture. Skeletal Radiol 2017; 46: 1193-1200.
- Muramatsu K, Saithna A, Watanabe H, Sasaki K, Yokosawa K, Hachiya Y, Banno T, Helito CP, Sonnery-Cottet B. Three-dimensional Magnetic Resonance Imaging of the Anterolateral Ligament of the Knee: An Evaluation of Intact and Anterior Cruciate Ligament-Deficient Knees From the Scientific Anterior Cruciate Ligament Network International (SANTI) Study Group. Arthroscopy 2018; 34: 2207-2217.
- Saithna A, Helito CP, Vieira TD, Sonnery-Cottet B, Muramatsu K. The Anterolateral Ligament Has Limited Intrinsic Healing Potential: A Serial, 3-Dimensional-Magnetic Resonance Imaging Study of Anterior Cruciate Ligament-Injured Knees From the SANTI Study Group. Am J Sports Med 2021; 49: 2125-2135.
- Van Dyck P, Clockaerts S, Vanhoenacker FM, Lambrecht V, Wouters K, De Smet E, Gielen JL, Parizel PM. Anterolateral ligament abnormalities in patients with acute anterior cruciate ligament rupture are associated with lateral meniscal and osseous injuries. Eur Radiol 2016; 26: 3383-3391.
- Oh YK, Lipps DB, Ashton-Miller JA, Wojtys EM. What strains the anterior cruciate ligament during a pivot landing? Am J Sports Med 2012; 40: 574-583.
- Yoon KH, Yoo JH, Kim K Il. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am 2011; 93: 1510-1518.
- Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med 2011; 39: 1439-1443.
- Viskontas DG, Giuffre BM, Duggal N, Graham D, Parker D, Coolican M. Bone bruises associated with ACL rupture: Correlation with injury mechanism. Am J Sports Med 2008; 36: 927-933.
- Ward P, Chang P, Radtke L, Brophy RH. Clinical Implications of Bone Bruise Patterns Accompanying Anterior Cruciate Ligament Tears. Sports Health 2022; 14: 585-591.
- Helito CP, Helito PVP, Leão RV, Demange MK, Bordalo-Rodrigues M. Anterolateral ligament abnormalities are associated with peripheral ligament and osseous injuries in acute ruptures of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2017; 25: 1140-1148.
- Lintin L, Chowdhury R, Yoong P, Chung SL, Mansour R, Teh J, McKean D. The anterolateral ligament in acute knee trauma: patterns of injury on MR imaging. Skeletal Radiol 2020; 49: 1765-1772.
- Lee DW, Kim JG, Kim HT, Cho SI. Evaluation of Anterolateral Ligament Healing After Anatomic Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2020; 48: 1078-1087.
- Marot V, Corin B, Reina N, Murgier J, Berard E, Cavaignac E. Femoral and tibial bone bruise volume is not correlated with ALL injury or rotational instability in patients with ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc 2021; 29: 900-906.
- Gracia G, Cavaignac M, Marot V, Mouarbes D, Laumonerie P, Cavaignac E. Epidemiology of Combined Injuries of the Secondary Stabilizers in ACL-Deficient Knees: Medial Meniscal Ramp Lesion, Lateral Meniscus Root Tear, and ALL Tear: A Prospective Case Series of 602 Patients With ACL Tears From the SANTI Study Group. Am J Sports Med 2022; 50: 1843-1849.
- Vincent JP, Magnussen RA, Gezmez F, Uguen A, Jacobi M, Weppe F, Al-Saati MF, Lustig S, Demey G, Servien E, Neyret P. The anterolateral ligament of the human knee: An anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 2012; 20: 147-152
- Shelbourne KD, Roberson TA, Gray T. Long-term Evaluation of Posterior Lateral Meniscus Root Tears Left In Situ at the Time of Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2011; 39: 1439-1443.
- Lee DW, Jang HW, Lee SR, Park JH, Ha JK, Kim JG. Clinical, radiological, and morphological evaluations of posterior horn tears of the lateral meniscus left in situ during anterior cruciate ligament reconstruction. Am J Sports Med 2014; 42: 327-335.
- Noyes FR, Barber-Westin SD. Treatment of meniscus tears during anterior cruciate ligament reconstruction. Arthroscopy 2012; 28: 123-130.
- Thompson WO, Fu FH. The meniscus in the cruciate-deficient knee. Clin Sports Med 1993; 12: 771-796.
- Fitzgibbons RE, Shelbourne KD. “Aggressive” Nontreatment of Lateral Meniscal Tears Seen During Anterior Cruciate Ligament Reconstruction. Am J Sports Med 1995; 23: 156-159.
- Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: A systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med 2014; 42: 921-926.
- DePhillipo NN, Moatshe G, Chahla J, Aman ZS, Storaci HW, Morris ER, Robbins CM, Engebretsen L, LaPrade RF. Quantitative and Qualitative Assessment of the Posterior Medial Meniscus Anatomy: Defining Meniscal Ramp Lesions. Am J Sports Med 2019; 47: 372-378.
- Cobby MJ, Schweitzer ME, Resnick D. The deep lateral femoral notch: An indirect sign of a torn anterior cruciate ligament. Radiology 1992; 184: 855-858.
- Losee RE, Johnson TR, Southwick WO. Anterior subluxation of the lateral tibial plateau. A diagnostic test and operative repair. J Bone Joint Surg Am 1978; 60: 1015-1030.
- Kanakamedala AC, Burnham JM, Pfeiffer TR, Herbst E, Kowalczuk M, Popchak A, Irrgang J, Fu FH, Musahl V. Lateral femoral notch depth is not associated with increased rotatory instability in ACL-injured knees: a quantitative pivot shift analysis. Knee Surg Sports Traumatol Arthrosc 2018; 26: 1399-1405.
To cite this article
Magnetic resonance imaging evaluation of anterolateral ligament injuries and associated lesions in acute anterior cruciate ligament tears
JOINTS 2023;
1: e676
DOI: 10.26355/joints_20239_676
Publication History
Submission date: 27 Mar 2023
Revised on: 01 Jun 2023
Accepted on: 10 Jul 2023
Published online: 04 Sep 2023