JOINTS 2023;
1: e756
DOI: 10.26355/joints_202310_756
Intra-articular subperiosteal osteoid osteoma of the talar neck mimicking impingement or bone marrow syndromes: report of 2 cases
Topic: Ankle
Category: Case report
Abstract
BACKGROUND: Two cases of a rare Subperiostal Osteoid Osteoma of the talar neck are reported. The purpose of these two case reports is to analyze and discuss its clinical and radiological presentation, and how it can mimic common foot and ankle painful syndromes.CASE PRESENTATION: Both cases were in young males with aspecific ankle pain and tenderness at the medial tibiotalar join line. Ankle MRI was inconclusive, and misleading diagnoses of anterior impingement and bone edema syndrome were performed by previous clinicians. Diagnosis of Subperiostal Osteoid Osteoma was confirmed after accurate symptoms and MRI review and after the execution of a SPECT-CT. The intra-articular position and proximity to the articular cartilage did not allow the execution of imaging-guided percutaneous techniques. Thus, arthroscopic removal was performed, with immediate pain relief and no recurrence.
CONCLUSIONS: Clinical-radiological presentation makes clinicians aware of the typical presentation of an intra-articular talar osteoid osteoma and assists in its challenging diagnosis and treatment.
Background
Originally described by Bergstrand1 in 1930 and framed as an anatomic-clinic entity by Jaffe2 in 1935, Osteoid Osteoma (OO) is a neoplasm that represents nearly 10-12% of all benign bone tumors1-3. The most frequently affected skeletal areas are represented by the diaphysis or metaphysis of long bones, followed by the talar localization (2-10% of all cases)4,5.
Characteristic symptomatology of an Osteoid Osteoma is a focal bone pain referred to as persistent, typically burdening with nocturnal acme, and sensitive to medical therapy with non-steroidal anti-inflammatory drugs (NSAIDs), especially salicylates. In the case of periarticular or intraarticular lesions, joint pain may occur with atypical presence of synovitis.
Due to its non-specific symptoms mostly characterized by pain, its diagnosis could be challenging, especially in uncommon and complex anatomical regions such as the foot and ankle. Moreover, the Subperiostal subtype of osteoid osteoma is a rarer form of the disease and usually occurs as a rounded mass in the soft tissue adjacent to the cortical bone. Considering the more common painful foot and ankle conditions such as anterior impingement or bone edema and the challenging imaging, Subperiostal Osteoid Osteoma could be easily missed, and its diagnosis and treatment could be delayed by 2 to 3 years since the symptom’s onset.
Another critical aspect of osteoid osteoma is its treatment: the gold standard is represented by CT-guided radiofrequency ablation, which, however, does not allow an adequate histological evaluation in a relevant percentage of the cases and could potentially create cartilaginous damage in the case of intra-articular Osteoid Osteoma. In this regard, arthroscopy can represent a precise and minimally invasive technique to remove the osteoma and explore the whole joint, addressing other eventual intra-articular lesions.
The purpose of the presentation of these two case reports of Subperiostal Osteoid Osteoma is to analyze and discuss its clinical and radiological presentation, and how it can mimic common foot and ankle painful syndromes such as anterior impingement and bone edema, in order to make sports doctors and surgeons of a possible differential diagnosis. Moreover, the efficacy of arthroscopic treatment is reported.
Case Report
Case 1
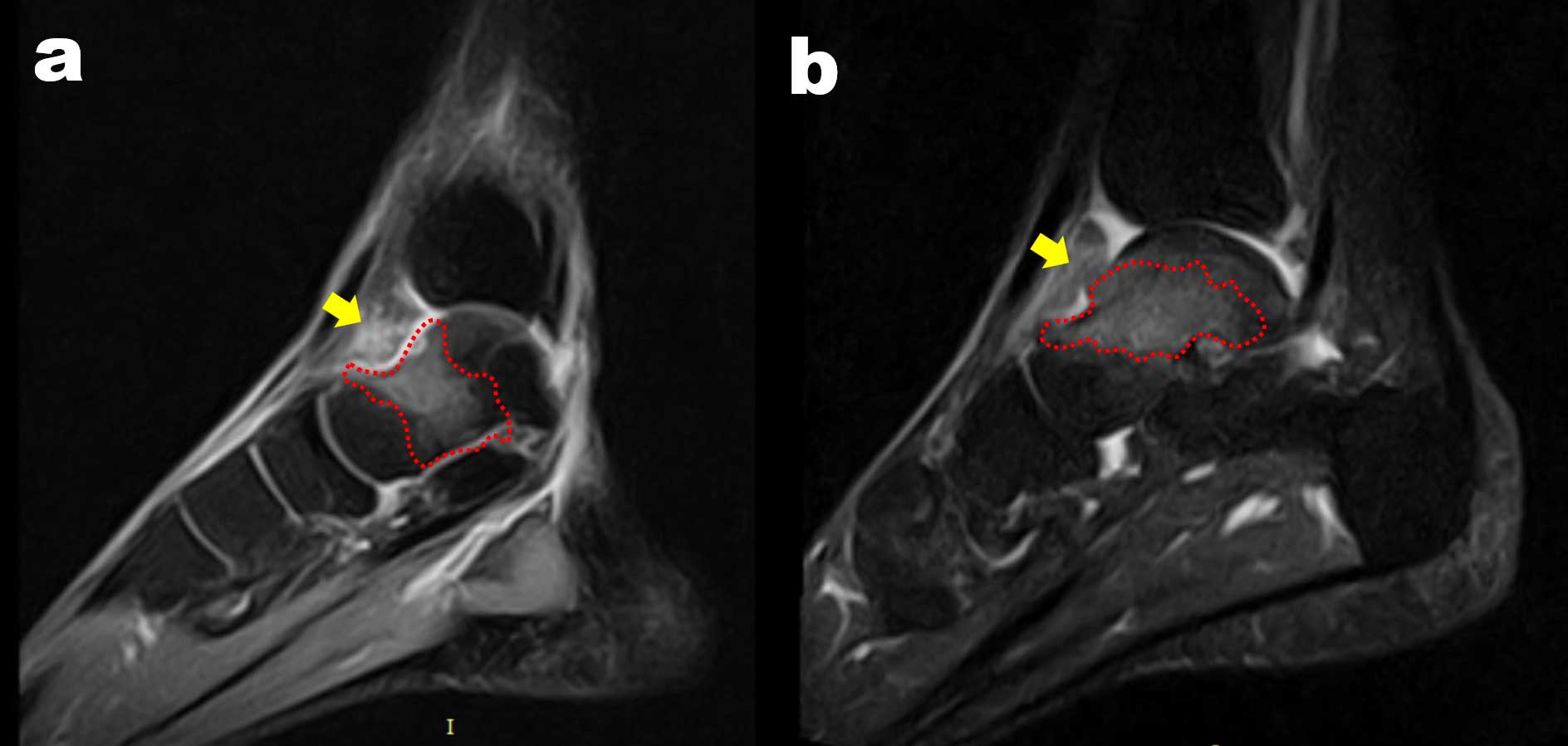
A 26-year-old male patient presented at our Department of Sports Medicine complaining of left ankle pain and limited range of motion, precluding sports participation and interference with normal daily life activities. At the interview, no relevant medical conditions were identified. The patient reported the onset of ankle pain after an inversion sprain occurred 3 years before, which was treated conservatively in another hospital. Due to persistent symptoms, the patient underwent an ankle MRI, where diffuse talar bone edema was noted (Figure 1a). No other abnormalities were reported by the radiologist, and the patient was treated with oral bisphosphonate for post-traumatic bone marrow edema syndrome.
After one other year, the patient was still symptomatic and underwent a new MRI where persistent bone marrow edema was still present (Figure 1b). Therefore, the patient was treated with another course of oral bisphosphonate, and physical therapy was prescribed, without success.
Figure 1. Case 1: The two sagittal cuts of two different pre-operative MRIs (a–b) performed at 1 year of distance show large and persistent bone edema (red dotted line) at the level of talar neck, and synovitis in the anterior joint space (yellow arrow). However, it is not possible to clearly identify the Osteoid Osteoma nidus.
After 3 years after the symptom onset, the patient presented at the attention of the Senior Author (A.G.). The symptoms reported were persistent pain, especially with ankle dorsiflexion and at night. The patient was unable to tolerate prolonged weight-bearing and abandoned any form of sports practice. Crutches were needed occasionally. At clinical examination, swelling of the ankle joint was experienced, especially at the level of the medial tibio-talar joint line. At palpation, an extremely painful area was identified medially to the anterior tibialis tendon. The pain was worsened with forced dorsiflexion, which was limited to a few degrees.
The previous imaging was reviewed, and an irregularity of the talar neck profile and synovitis were noted medially, corresponding to the area of maximum pain (Figure 1). A CT scan was performed, and a round formation of nearly 8 mm was noted (Figure 2a, b) and considered compatible with the diagnosis of Subperiostal Osteoid Osteoma. Bone scintigraphy was performed, which further strengthened the diagnostic suspect. The patient was thus scheduled for arthroscopic excision, biopsy, synovectomy, and bone spur removal.
Figure 2. Case 1: In the sagittal (a) and axial (b) view of the CT scan, it is possible to appreciate the nidus of the subperiosteal Osteoid Osteoma (red arrow) at the junction between talar cartilage and talar neck.

Case 2
A 24-year-old male patient presented at our Department of Sports Medicine complaining of left ankle pain impairing normal daily life activities. At the interview, no relevant medical conditions were identified. The patient reported an insidious onset of the pain, with an inability to perform any sports activity, including the habitual sports practice of recreational soccer. An MRI was performed in another hospital, where anterior compartment synovitis, consistent with fibrous impingement, was reported (Figure 3a, b). The patient was thus treated with physical therapy and strengthening, with temporary symptoms improvement. After 2 years of therapy, the patient was still symptomatic, unable to perform any sports activity, and not satisfied with his quality of life.
When the patient came to the attention of the Senior Author (A.G.), symptoms were still present, and after a deep interview, the patient described the peak of pain during the night and in early afternoon. At clinical examination, the ankle was swollen medially to the anterior tibialis, with extreme pain at palpation and with forced ankle dorsiflexion.
Figure 3. Case 2: The T2 sagittal cut of the pre-operative MRI shows a large bone edema (red dotted line) at the level of talar neck and synovitis in the anterior joint space (yellow arrow) (a). The T1 sagittal cut of the same MRI shows an unspecific irregular signal at the level of the talar neck (red arrow), initially interpreted as fibrotic tissue (b).
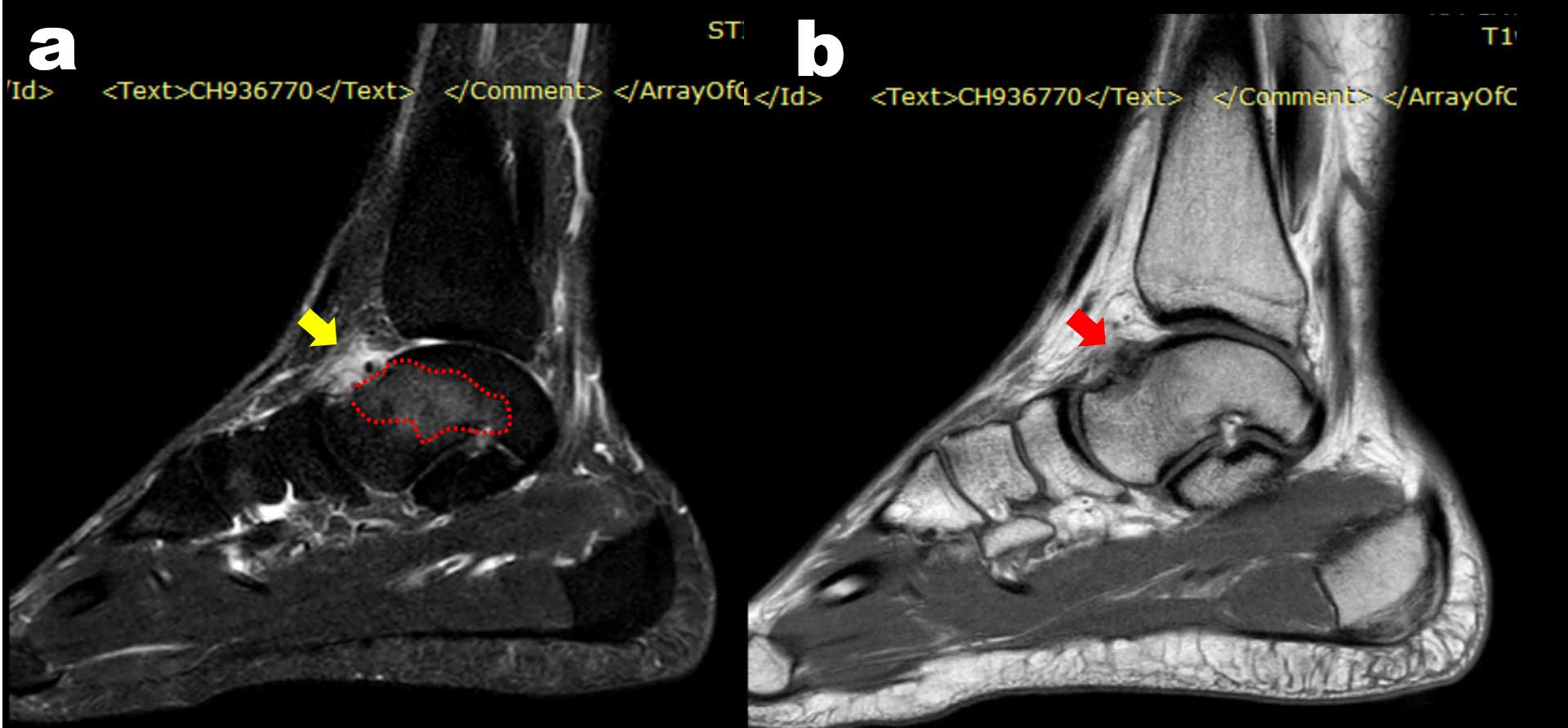
The previous MRI was reviewed, and an irregularity of the talar neck profile and synovitis were noted medially, corresponding to the area of maximum pain; moreover, a diffuse edema of the talar neck was noted as well (Figure 3a, b). A CT scan was performed, which showed a round formation of nearly 6 mm (Figure 4a, b). With the clinical suspect of an intra-articular Subperiostal Osteoid Osteoma, a bone scintigraphy was performed, confirming the diagnosis, detecting a round and well-defined signal at the level of the bone irregularity (Figure 5). The patient was thus scheduled for arthroscopic excision, biopsy, and synovectomy. Both patients were treated according to the standard of care at our institution; no experimental treatments were performed requiring a specific study enrollment, and consent was given for the collection of radiological and arthroscopic images.
Figure 4. Case 2: In the sagittal (a) and axial (b) view of the CT scan it is possible to appreciate the nidus of the subperiosteal Osteoid Osteoma (red arrow) at the junction between talar cartilage and talar neck.
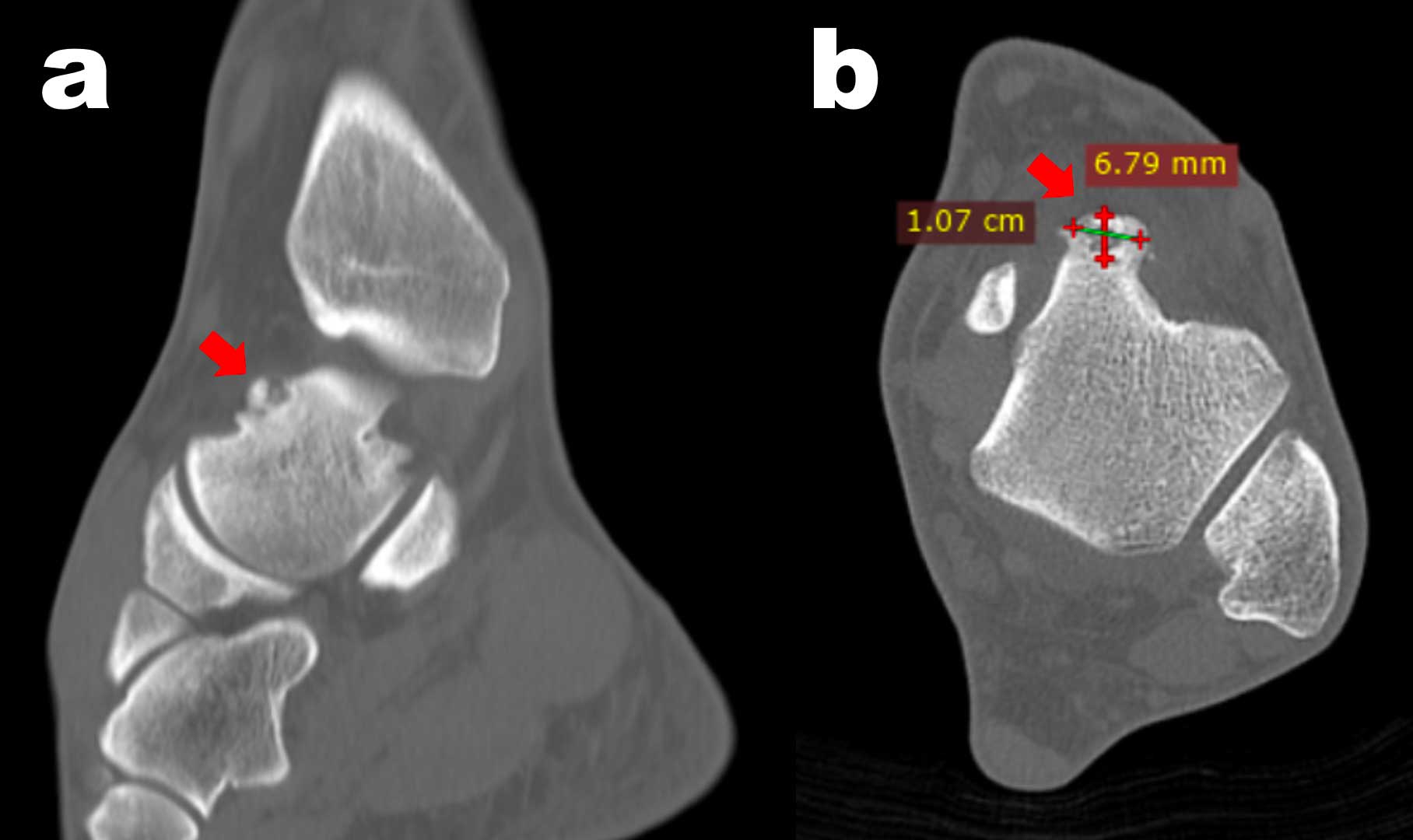
Figure 5. Case 2: The SPECT-CT shows a well-defined round-shape uptake at the level of the talar neck in either axial, sagittal or coronal view, corresponding to the most painful location at physical examination.

Treatment and Outcomes
Both patients were operated on by the same Senior Author (A.G.), under spinal anesthesia. Patients were positioned supine with a sandbag under the ipsilateral hemipelvis. A standard arthroscopic setting with anterolateral and anteromedial portals was used, after marking anatomical landmarks (anterior tibialis tendon, medial and lateral malleolus, joint line superficial peroneal nerve) with a sterile surgical pen. With the ankle in dorsiflexion and the scope in the anteromedial portal, diffuse synovitis was noted (Figure 6a); thus, a careful synovectomy with the shaver blade was performed until it was possible to explore the tibiotalar joint. Moving the scope toward the medial portion of the talus, a round cherry-red formation with an aspect similar to cancellous bone and a dimension of nearly 10 mm was immediately noted in Case 1 (Figure 6b). In Case 2, a round formation of sclerotic bone was instead present. While performing ankle dorsiflexion, it was possible to note the impingement of the mass within the tibiotalar joint. In Case 1, the mass was removed with graspers (Figure 6c), trying to obtain a large specimen for histological evaluation (Figure 4), which later confirmed the diagnosis of Osteoid Osteoma. In Case 2, it was necessary to remove a small layer of bone with a motorized burr in order to access the nucleus of the Osteoid Osteoma and proceed to its removal. The resection was continued using a 4.5 mm shaver, trying to remove the remaining pathologic tissue within the bone cavity (Figure 6d), and gently completed with a 5 mm curette, until healthy bone with normal trabeculae was obtained all around the removed neoformation (Figure 6e). Finally, a 4.5-mm burr was used to excise the sclerotic rim and all excessive bone at the margins of the nidus, regularizing the edges of the remaining cavity. The complete nidus excision was confirmed macroscopically (Figure 6f). Considering its proximity with the nidus, the anterior tibial lip was debrided as well with curette and shaver, until cancellous bone was noted. After all pathologic tissue was removed (Figure 7), the 4.5-mm shaver was used to complete a partial synovectomy, especially in the medial gutter and anterior chamber, until a normal range of motion was reached. The procedure was completed by performing hemostasis with the Vapor device (VAPR VUE™ Radiofrequency Electrode System – DePuy Mitek, Inc, Raynham, USA), which was used to cauterize the bone around the osteoid osteoma in order to destroy any remaining pathology cells trying to avoid recurrence. Joint lavage was performed, and the arthroscopic portals were closed with 3.0 VICRYL™ suture (ETHICON, Jhonson & Jhonson Medical, Cincinnati, USA).
Figure 6. Arthroscopic views from the anterolateral portal: first, it is possible to appreciate diffuse synovitis (a) and a red cherry-like neoformation at the level of the talar neck, just below the cartilage margin (b). The pathologic tissue is removed with a grasper (c), exposing the bone nidus (d). After the lesion debridement, a curette is used to remove any remaining pathological tissue (e). At the end of the procedure, no impingement is present during all ranges of motion (f).

Weight-bearing was allowed as tolerated with the use of crutches and wearing a Walker boot (XCELTRAX™ STANDARD – Enovis, Duesseldorf, Germany) for 15 days, until the removal of sutures. Range of motion exercises, especially dorsiflexion and triceps muscle stretching, were initiated immediately.
Both patients reported being pain-free since the first post-operative week. They returned to play sports 6 weeks after the procedure and reported improvement of ankle mobility. The patients were satisfied with the procedure and were able to return to normal daily life activities and desired sports without discomfort. No recurrences were reported during the first 12 months.
Figure 7. Macroscopic aspect of the Osteoma Osteoid fragment obtained after the debridement.

Discussion
The most important lessons learned from these two case reports are that Subperiosteal Osteoid Osteoma could mimic common painful foot and ankle syndromes such as anterior impingement and bone edema, resulting in delayed diagnosis, and that arthroscopic treatment of this condition can be effective, with immediate symptoms relief, rapid recovery and absence of recurrence.
In the anterior ankle impingement syndrome, the cause of pain is hypothesized not to be the talotibial osteophytes at the anterior part of the ankle joint, but the inflamed soft tissue impingement that occurs between the osteophytes. Clinically, the typical patient is a young athlete with a history of recurrent inversion sprains with vague, chronic anterior ankle pain, swelling after activity, and limited dorsiflexion6.
Bone marrow edema syndrome is characterized by extremity pain of unknown etiology. Symptoms may include sudden or gradual onset of swelling and pain at rest or during activity, usually at night. This syndrome mostly affects middle-aged men and younger women who have pain in the lower extremities. The bone marrow edema pattern on MRI is characterized by decreased signal in T1-weighted images and increased signal on fat-suppressed T2-weighted images or short tau inversion recovery (STIR) images7.
Several aspects make the diagnosis challenging. First of all, the aspecific clinical symptoms characterized by pain and ankle tenderness represent the most controversial aspect. In fact, the two patients described here were diagnosed with anterior impingement and bone edema syndrome, respectively. However, when a careful patient interview was performed, uncommon features could be identified, such as night pain, severe pain with ankle dorsiflexion, symptoms not strictly related to activity, and no history of major trauma or repetitive microtraumas. All these aspects should raise suspicion in the diagnosis and move the clinician to perform a deeper radiological assessment.
The other controversial aspect, and maybe the most important one, is the imaging; in fact, in both cases, the ankle MRI was misleading, and the first treating clinicians were not able to formulate the correct diagnosis. In fact, in one case, the hyperintense signal in the talar neck was interpreted as post-traumatic bone edema syndrome, while in the other case, it was wrongly attributed to an impingement condition. If carefully assessed, the bone edema presented an unusual location and peculiar characteristics: in fact, it involved the talar neck and did not extend to the subchondral region of the talar dome, thus making the diagnosis of osteochondral overload or initial OCD not likely. Moreover, the lack of repetitive micro-traumas in the patient’s history (running, heavy work, military, etc.) and the lack of a fracture line in both MRI and CT could exclude the diagnosis of a talar neck stress fracture. Another element of suspicion, despite not easily identified, was the anterior synovitis. Differently, the Osteoid Osteoma nidus was not clearly visible in standard MRI, especially in those with low field. In fact, the Subperiosteal Osteoid Osteoma represents a rarer form and usually occurs as a rounded mass in the soft tissue adjacent to the bone cortical, which results in excavation, and for this reason, the surrounding typical sclerosis is usually absent. In this regard, CT can be a more appropriate tool to assess the shape of the lesion, even if the nidus can be overlooked even by radiologists, as in these two cases. It is, therefore, of paramount importance to pay extreme attention in the imaging to the area corresponding to the maximum pain at palpation. Finally, when the suspect of Subperiostal Osteoid Osteoma is concrete, the diagnosis can be confirmed with the SPECT-CT.
A correct and prompt diagnosis is important because it can allow early treatment, preventing patients from spending years of not-controlled pain at a young age, and compromising their daily life, sports, and work.
Some consideration should also be made for the treatment: it is fundamental to plan an accurate procedure to completely remove the mass and avoid the spreading of the disease. In fact, a case of recurrence was previously described8 when an ankle arthroscopy for synoviectomy was performed without pre-operatively recognizing the disease, and thus without carefully planning a safe and complete removal of the neoplastic lesion. Conversely, when a correct diagnosis is formulated pre-operatively, the recurrence rate after arthroscopic removal is reported9 to be lower than 5%. This is important since ankle arthroscopy represents a minimally invasive and effective treatment, that allows early weight-bearing and mobilization, with immediate pain relief. In fact, both patients reported immediate disappearance of pain since the first days after surgery, especially during the night, and both reported immediate discontinuance of NSAID use. Another advantage of arthroscopic removal with respect to the surgical en-bloc resection considered the only solution in past decades10,11, is the easier localization of the lesion, resulting in the possibility of a smaller and more precise excision of healthy bone tissue, avoiding the risk of weakening the bone segment and the need bone grafting and prolonged post-operative immobilization. Arthroscopic removal of talar neck Subperiostal Osteoid Osteoma also has advantages with respect to percutaneous Radiofrequency thermoablation (RFA)12,13. In fact, despite Radiofrequency thermoablation (RFA) represents an option whose safety and efficacy have now been demonstrated by numerous studies14-19, it requires precise targeting with a solid intraosseous positioning of the trocar, which may be difficult in the intra-articular localizations. Moreover, the possible heat dispersion from the electrode can damage the adjacent cartilaginous tissue in case of intra-articular lesions. Finally, percutaneous treatment does not allow to perform an adequate synovectomy and address other possible intra-articular abnormalities.
Thus, the arthroscopic excision of intra-articular osteoid osteoma is nowadays a surgical technique of considerable interest, although it is still poorly described. It is thus important to keep in mind that talar neck subperiostal Osteoid Osteoma can be immediately visible intra-articular as a cherry-red formation of cancellous bone like in the first described case or can be identified with difficulty only after a limited debridement of the surrounding sclerotic bone like in the second case. In this regard, pre-operative planning to identify the lesion according to arthroscopic landmarks is fundamental. In the present cases, the mass was noted to impinge with the anterior tibial lib during ankle dorsiflexion; this feature motivated the extreme pain experienced by the patients, especially with forced dorsiflexion and palpation of the medial joint line. From the technical point of view, initial mass removal was performed with a grasper and without suction tools, in order to obtain sufficient material for histological evaluation. Moreover, extreme care was used not to disseminate pathological tissue within the joint. Therefore, curette and suction were used to gradually remove a small amount of tissue. Vapor was used as well to cauterize the nidus and possible remaining cells.
Conclusions
Young patients with ankle pain, medial joint line tenderness, and pain at dorsiflexion at clinical examination, and with talar neck bone edema without clear stress fractures or Osteochondral Lesions, anterior synovitis, and superficial abnormalities of the talar neck should be suspected as Subperiostal Osteoid Osteoma. Its removal through ankle arthroscopy is possible, safe and effective; however, precise preoperative planning to proper identify the location and to avoid cells dissemination is mandatory.
Conflict of Interest
Nothing to declare.
Funding
None.
ORCID ID
Alberto Grassi: 0000-0003-4236-1798
Massimiliano Mosca: 0000-0002-3283-8735
Silvio Caravelli: 0000-0001-9092-225X
Simone Massimi: 0009-0001-8604-2265
Anna Pagano: 0009-0001-3402-7530
Stefano Zaffagnini: 0000-0002-2941-1407
Data Availability
Data are available from the corresponding author.
Informed Consent
All subjects provided written informed consent for inclusion before they participated in the study.
Ethics Approval
Not applicable.
References
1. Bergstrand H. Über eine eigenartige, wahrscheinlich bisher nicht beschriebene osteoblastische Krankheit in den langen Knochen der Hand und des Fusses. Acta Radiol 1930; 11: 596.
2. Jaffe HL. Osteoid osteoma: a benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg. 1935; 31: 709-728.
3. Kransdorf MJ, Stull MA, Gilkey FW, Moser Jr RP. Osteoid osteoma. Radiographics 1991; 11: 671-696.
4. Golding JSR. The natural history of osteoid osteoma with a report of twenty cases. J. Bone Joint Surg 1954; 36: 218-229.
5. Jordan RW, Koç T, Chapman AWP, Taylor HP. Osteoid osteoma of the foot and ankle – a systematic review. Foot Ankle Surg 2015; 21: 228-234.
6. Tol JL, van Dijk CN. Anterior Ankle Impingement. Foot and Ankle Clinics 2006; 11: 297-310.
7. Mirghasemi SA, Trepman E, Sadeghi MS, Rahimi N, Rashidinia S. Bone Marrow Edema Syndrome in the Foot and Ankle. Foot Ankle Int. 2016; 37:1364-1373.
8. Dubuc JE, Docquier PL, Schubert T, Galant C, Malghem J. Diagnosis failure led to the recurrence of an intra-articular osteoid osteoma at the talus neck after arthroscopic excision. Foot Ankle Surg 2014; 20: 40-42.
9. Ge SM, Marwan Y, Addar A, Algarni N, Chaytor R, Turcotte RE. Arthroscopic Management of Osteoid Osteoma of the Ankle Joint: A Systematic Review of the Literature. J Foot Ankle Sur 2019; 58: 550-554.
10. Yildiz Y, Bayrakci K, Altay M, Saglik Y. Osteoid osteoma: the results of surgical treatment. Int Orthop 2001; 25: 119-122.
11. Boscainos PJ, Cousins GR, Kulshreshtha R, Oliver TB, Papagelopoulos PJ. Osteoid osteoma. Orthopedics 2013; 36: 792-800.
12. Roger B, Bellin M, Wioland M, Grenier P. Osteoid osteoma: CT-guided percutaneous excision confirmed with immediate follow-up scintigraphy in 16 outpatients. Radiology 1996; 201: 239-242.
13. De Berg JC, Pattynama PM, Obermann WR, Bode PJ, Vielvoye GJ, Taminiau AH. Percutaneous computed tomography-guided thermocoagulation for osteoid osteomas. Lancet 1995; 346: 350-351.
14. Pinto CH, Taminiau AHM, Vanderschueren GM, Hogendoorn PCW, Bloem JL, Obermann WR. Technical considerations in CT-guided radiofrequency Thermal ablation of osteoid osteoma: Tricks of the trade. AJR 2002; 179: 1633-1642.
15. Lindner NJ, Ozaki T, Roedl R, Gosheger G, Winkelmann W, Wortler K. Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Joint Surg Br 2001; 83: 391-396.
16. Woertler K, Vestring T, Boettner F, Winkelmann W, Heindel W, Lindner N. Osteoid osteoma: CT-guided percutaneous radiofrequency ablation and follow-up in 47 patients. J Vasc Interv Radiol 2001; 12: 717-722.
17. Laus M, Albisinni U, Alfonso C, Zappoli FA. Osteoid osteoma of the cervical spine: surgical treatment or percutaneous radiofrequency coagulation? Eur Spine J 2007; 16: 2078-2082.
18. Sung KS, Seo JG, Shim JS, Lee YS. Computed-tomography-guided percutaneous radiofrequency thermoablation for the treatment of osteoid osteoma – 2 to 5 years follow-up. Int Orthop 2007; 22.
19. Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am 1998; 80: 815-821.
To cite this article
Intra-articular subperiosteal osteoid osteoma of the talar neck mimicking impingement or bone marrow syndromes: report of 2 cases
JOINTS 2023;
1: e756
DOI: 10.26355/joints_202310_756
Publication History
Submission date: 29 Aug 2023
Revised on: 11 Sep 2023
Accepted on: 05 Oct 2023
Published online: 27 Oct 2023